That sprinkle of cinnamon in your coffee or oatmeal? Probably harmless. But taken as a supplement, it could change how your body processes prescription drugs, new research suggests.
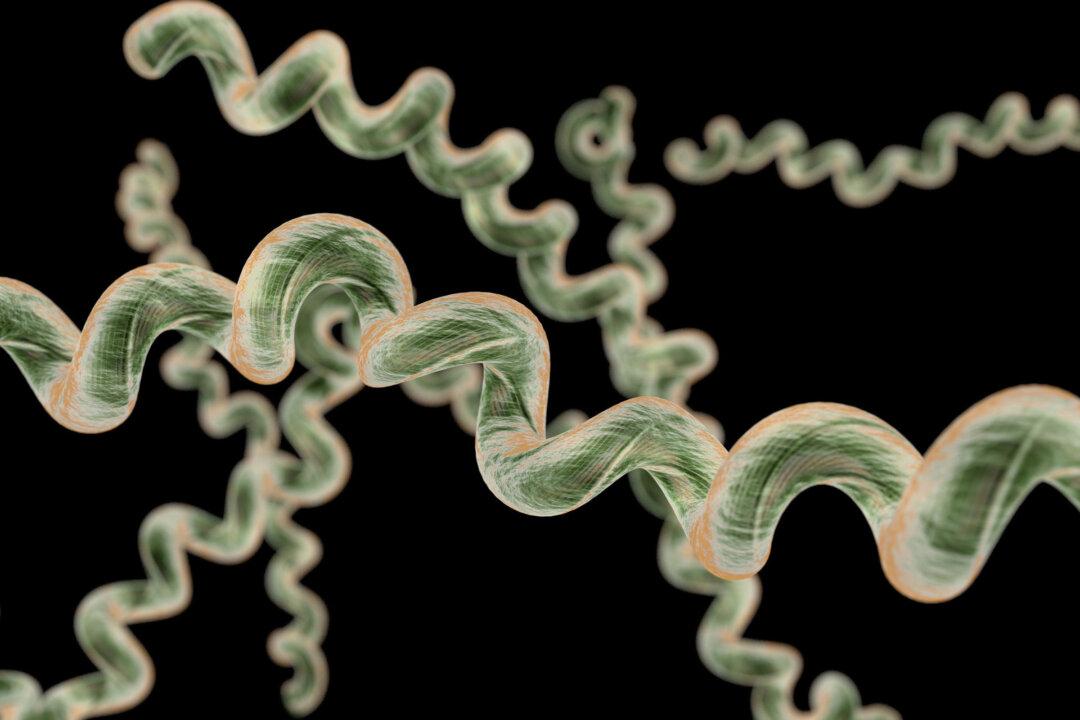
Cinnamaldehyde, the compound behind cinnamon’s signature flavor and scent, can interfere with how the body processes medications. The recent study on human liver and gut cells found that at high concentrations, the compound may speed up drug metabolism, clearing medications before they can take full effect.
What Researchers Discovered
In a study from the University of Mississippi, published in Food Chemistry: Molecular Sciences, researchers found that cinnamaldehyde can switch on certain receptors in the body—known as PXR and AhR—that may cause the body to clear medications too fast, which can cause them to reduce their effectiveness.At concentrations above 270 micrograms per milliliter, which would be reached only through taking high-dose supplements, cinnamaldehyde activated these receptors, acting like gatekeepers, telling the body how quickly to break down and eliminate medications.
Researchers say that this could be a concern for people taking certain medications—particularly drugs metabolized by the liver enzymes CYP2C9 and CYP1A2, such as some blood thinners, diabetes drugs, antidepressants, and anti-inflammatory drugs.
“Cinnamon and cinnamon-based supplements are quite safe when used in moderation,” Gurley said. “The likelihood that cinnamaldehyde poses any risk for clinically relevant drug interactions is quite low.”
The researchers found no changes in PXR activity at lower levels of cinnamaldehyde (up to 20 micrograms per milliliter), suggesting that everyday use—like those typically used in cooking—is unlikely to be a problem.
“It is okay to consume cinnamon in food or take it as a supplement in moderation,” Shabana Khan, a principal scientist at the university’s National Center for Natural Products Research and co-author of the study, told The Epoch Times in an email. Health concerns, however, can arise when supplements are used in high doses or for long periods—especially without a doctor’s knowledge.
Know Your Cinnamon
Cinnamon is used in several forms, each with varying levels of risk.Ground cinnamon, the kind you likely have in your spice rack, is used in cooking and baking, and up to a teaspoon is considered safe. Cinnamon oil, often used in foods and personal care products, poses little risk in small amounts. However, supplements, which can contain anywhere from 500 to 1,000 milligrams per dose, can be more concentrated and potentially interfere with medications when taken regularly.
Labels don’t always list the type of cinnamon used; unless otherwise stated, it’s mostly like going to be cassia. You can also contact the manufacturer for clarification, especially if you are taking cinnamon in supplement form.
Apart from cinnamaldehyde, cinnamon also contains coumarin, a naturally occurring blood thinner.
“Cassia cinnamon, often sourced from regions like Southern China, contains significantly higher levels of coumarin and is a potent blood thinner compared to true cinnamon (Cinnamomum verum) from Sri Lanka,” study co-author Amar Chittiboyina, associate director at the National Center for Natural Products Research, told The Epoch Times in an email.
“We strongly advise individuals currently taking blood thinners who are considering incorporating cinnamon into their daily routine to consult with their primary healthcare physician,” Chittiboyina said.
Other Competing Foods and Herbs
Cinnamon isn’t the only natural ingredient that can interact with medications. Common foods and herbs can affect how drugs are absorbed or broken down—something to keep in mind if you take medication regularly.Several herbs and supplements have also been linked to well-documented drug interactions, according to Gurley. St. John’s Wort, often used for mild depression, can reduce the effectiveness of medications like antidepressants, birth control pills, and antivirals by speeding up liver enzyme activity.
Goldenseal may slow down drug metabolism of certain statins, antihistamines, and sedatives, increasing drug levels in the body. And licorice root—unless it’s had the glycyrrhizin compound removed—can raise blood pressure and interfere with blood pressure medications.
“Our best advice is to talk to a health care provider before using any supplements along with prescription medicine,” Khan said.