Lupus is sometimes referred to as a “non-lethal cancer.” Recently, a woman from China, overwhelmed by the physical and emotional toll of the disease, traveled to Switzerland to seek assisted suicide, sparking widespread discussion online.
The 43-year-old Shanghai woman had been diagnosed with systemic lupus erythematosus at age 20. After a series of flare-ups, she suffered from kidney failure and was having to undergo dialysis three times a week. The case of the woman—known as “Shabai” but later identified on the LinkedIn social media platform as Elizabeth Zheng, a Shanghai professional with an MBA—sparked an online debate in China. In a goodbye video uploaded on Oct. 23, the woman stated her wish not to be a burden to her 80-year-old father and her plans to die by euthanasia in Switzerland on the following day.
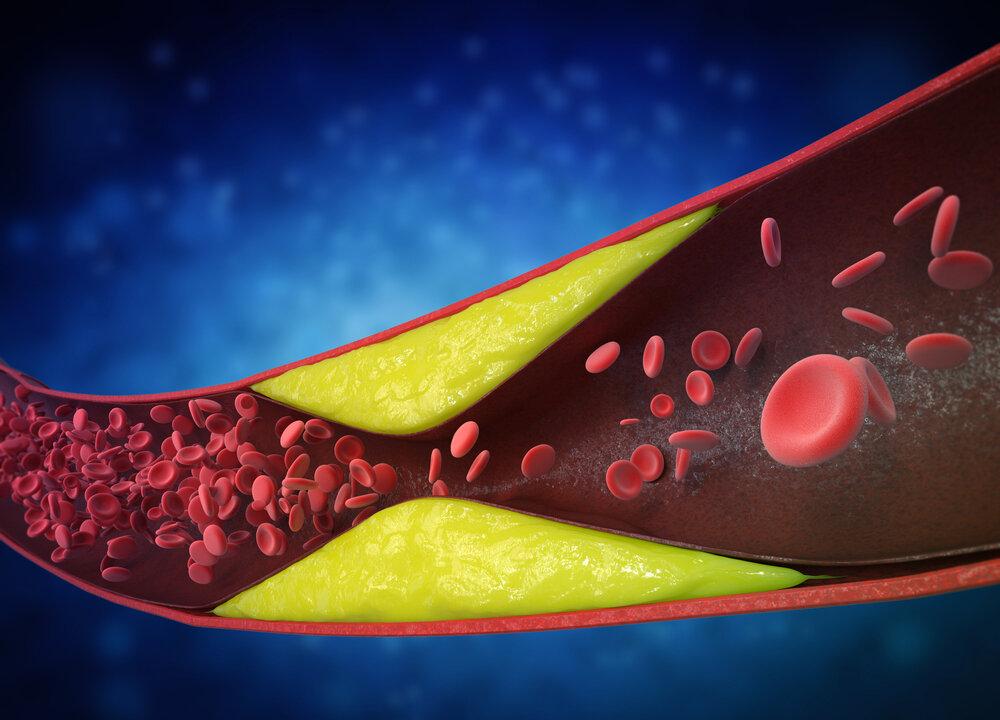
Lupus, formally known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the immune system mistakenly attacks the body’s own tissues. This leads to widespread inflammation that can affect the skin, joints, organs, and even the brain.
The disease’s onset is driven by a combination of genetic and environmental factors, and understanding these factors is crucial to improving the quality of life of those diagnosed. Increasing awareness of self-care strategies and medical options could greatly enhance the well-being of lupus patients. Certain self-care strategies may help alleviate its symptoms.
Genetic Factors
The underlying mechanisms of lupus onset are highly complex. Research highlights a blend of genetic predispositions and environmental triggers that play pivotal roles in the development of the disease.For instance, having a close family member, such as a parent or sibling, with lupus increases the risk of developing the condition, but it does not guarantee it. Specific genetic variations linked to an increased risk of autoimmune responses can affect the way that the immune system operates. While some of the cause may be genetic, this is only one piece of a much larger puzzle.
Epigenetic Mechanisms
Epigenetics explores how environmental factors influence gene expression, helping to explain why some people with lupus-associated genes do not develop the disease—unless specific environmental “switches” activate those genes.Environmental factors, such as sun exposure, infections, and hormonal changes, can be just as impactful as genetic predispositions.
Higher Incidence in Women
The incidence of lupus is higher in women, and researchers suggest that this may be linked to the X chromosome. Women have two X chromosomes, while men have only one.Impact on Brain and Mental Health
The impact of lupus extends beyond physical symptoms. Many patients experience cognitive symptoms such as brain fog, memory loss, and difficulty concentrating, which can make daily life and work significantly more challenging. In severe cases, these symptoms may lead to an inability to live independently.Emotional support plays a crucial role in managing lupus because it can help reduce stress and improve emotional well-being, contributing to better disease management.
Conversely, stress can exacerbate symptoms in lupus patients, necessitating a comprehensive approach to care that includes support networks.
Self-Care Strategies
For people with lupus or other autoimmune diseases, the following strategies may help improve symptoms and enhance overall well-being:Adopt an Anti-Inflammatory Diet
Omega-3-rich foods, such as salmon and flaxseed, help reduce inflammation by regulating inflammatory signaling pathways. It is also advisable to limit the intake of processed foods, sugar, and trans fats, as they can increase inflammation.Prioritize Quality Sleep
Regular, high-quality sleep is crucial for managing lupus. For those who struggle to fall asleep, practices such as deep breathing, meditation, or light stretching before bed can help relax both the body and mind.Engage in Moderate Exercise
Regular physical activity helps maintain joint flexibility and improves mood. Low-impact exercises such as walking, swimming, or yoga are ideal, while strenuous activities should be avoided.Limit Sun Exposure
Many lupus patients are sensitive to sunlight. To minimize UV exposure, use sunscreen, wear sunglasses, and opt for protective clothing when outdoors. However, reduced sun exposure can lead to vitamin D deficiency, making supplementation with vitamin D3 and K2 important.Focus on Mental Health
Depression and anxiety are common among lupus patients, underscoring the importance of psychological therapy as part of overall care.While these conditions may not be directly caused by lupus, the epigenetic factors contributing to lupus may also play a role in the development of depression, anxiety, obsessive-compulsive disorder, and other mental health conditions.
Summary
Lupus is a multifaceted disease influenced by genetic, environmental, and familial factors. It affects physical health, brain function, and mental well-being. Fortunately, there are ways to manage and possibly improve the condition, including lifestyle changes, self-care, mental health support, and appropriate medical treatments.Lupus is not an incurable “non-lethal cancer” but rather a chronic condition that can be effectively managed. Even with a lupus diagnosis, it is important to remain hopeful and avoid feelings of despair or thoughts of giving up.
For those living with the disease, remember that you are not alone. Seeking support, managing triggers, maintaining open communication with your family, and working closely with professionals to better understand the disease can all have a profoundly positive impact on your path to recovery.