A questionable green light from the U.S. Food and Drug Administration (FDA). Medical experts left confused and concerned.
This is the story surrounding brexpiprazole, branded as Rexulti: the first antipsychotic approved to treat agitation in Alzheimer’s patients despite alarmingly high death rates and poor results in clinical trials.
Watchdog Group Flags Dangers as FDA OKs Alzheimer’s Drug
In an open letter (pdf) from May 3, Nina Zeldes, who has a doctorate in medical anthropology and is a drug safety advocate and researcher for Public Citizen, a consumer advocacy organization, urged the FDA to reject the drug manufacturer’s bid. She argued that the drug has no meaningful benefits and increases patients’ risk of harm.Approving ineffective drugs erodes public trust and gives false hope to families of Alzheimer’s patients, Ms. Zeldes wrote. Patients need to trust that FDA-approved drugs are safe and effective, she added.
Ms. Zeldes also noted that up to 21 percent of nursing home residents already receive risky antipsychotics, citing a New York Times investigation. According to Ms. Zeldes, approving brexpiprazole could increase the use of these potentially deadly drugs.
What Did the Clinical Trials Really Show?
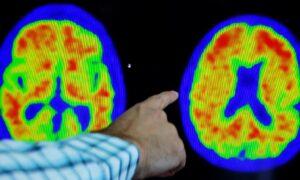
The efficacy of drugs for treating Alzheimer’s dementia is based on a scale called the Cohen-Mansfield Agitation Inventory (CMAI) (pdf) that measures 29 behaviors. Caregivers assign a score of 1 to 7 for each statement for a total score of 29 to 203. Some behaviors listed on the scale include how often a patient:- Hits, kicks, and screams.
- Is restless or paces aimlessly.
- Screams or curses.
- Repeatedly asks the same question.
- Complains or is excessively negative.
New Alzheimer’s Drug Joins Ranks of Risky Antipsychotics
A “boxed warning” is considered the highest safety-related warning issued by the FDA, intended to let the public and prescribers know a drug has been found to be linked with increased mortality. Brexpiprazole carries this warning, as do several other commonly prescribed antipsychotics.Results from studies on brexpiprazole were similar to results from earlier trials of antipsychotics in patients with Alzheimer’s, Lon Schneider, professor of psychiatry, neurology, and gerontology at the Keck School of Medicine at the University of Southern California, noted in the BMJ paper. “There are the same small points of difference on the [CMAI scale] that you see with every other drug,” he said.
Why Did It Get Approved Anyway?
Robert Whitaker, a renowned medical and investigative journalist and author of the BMJ paper, wrote that advocacy groups are the main drivers behind the FDA’s concession despite the drug’s potential significant medical and societal impacts. For example, Mr. Whitaker suggested alleged pressures came from organizations including the Alliance for Aging Research, Leaders Engage on Alzheimer’s Research (LEAD), Us Against Alzheimer’s, and the Alzheimer’s Association, all of whom “welcomed the decision” to approve the drug.“Antipsychotic medications are especially dangerous among the nursing home population because of their potentially devastating side effects, including death,“ a U.S. Centers for Medicare and Medicaid Services (CMS) spokesperson said in the paper. ”We cannot speak to the hypothetical future use of brexpiprazole; however, CMS will continue its efforts to reduce the prescribing of unnecessary antipsychotics in nursing homes.”