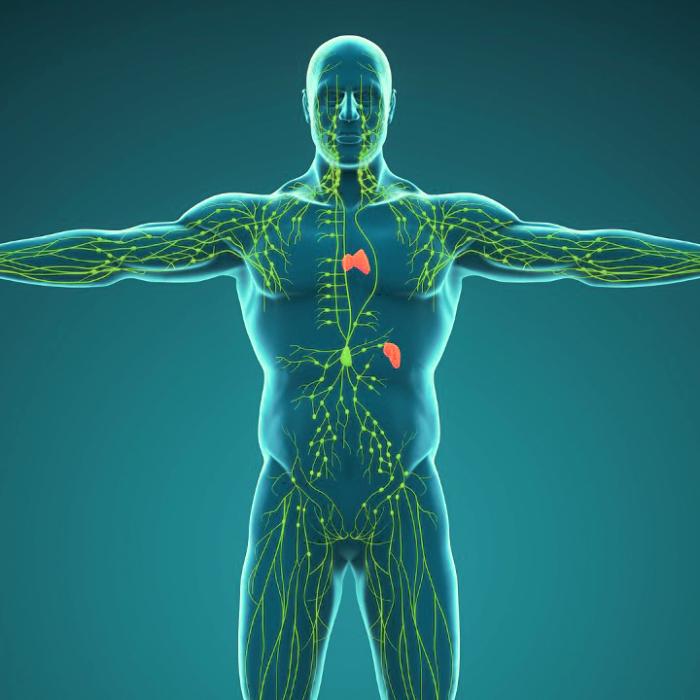
You may be amazed by how many types of immune cells your body has and how well they work together. You may also wonder where those immune cells are created and may be surprised to learn that they originate in the bone marrow.
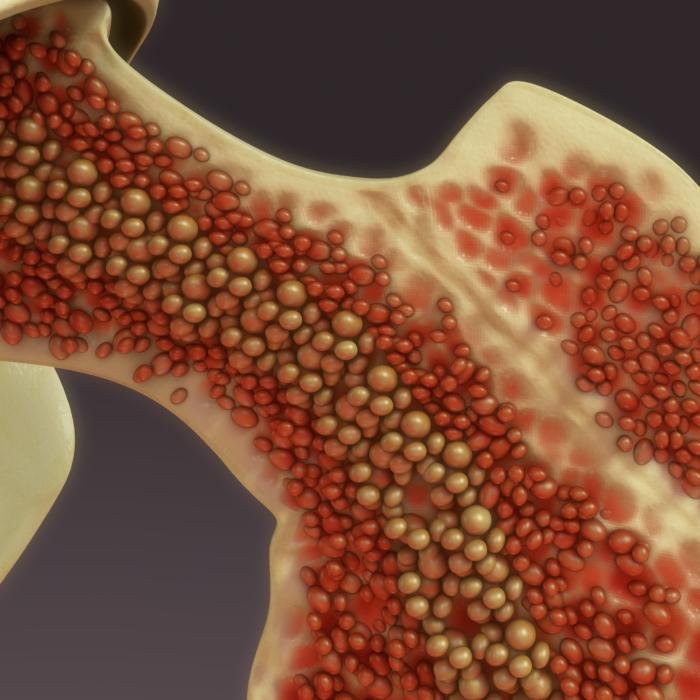
Picture a bustling city inside your bones, where billions of cells work tirelessly to create the building blocks of life, including blood. Welcome to the municipality of bone marrow!
Bone marrow is a soft and vital tissue responsible for the continuous production of the blood cells that nourish and protect the body. It has essential functions and a remarkable structure, but surprising new research reveals there are alternative sources of blood production.

Critical Role of Bone Marrow in Immunity and Blood Generation
Constituting about 4 percent of our body weight, bone marrow is a soft, jelly-like tissue built upon long trabeculae, which are beam-like structures. Although highly vascular like the spleen, another blood production organ, our bone marrow enjoys the protection of a hard outer shell of bone.There are two types of bone marrow: red and yellow. Red bone marrow is the “active” factory. Yellow blood marrow is mainly composed of fatty tissue and is normally dormant.
The Roles of Red and Yellow Bone Marrow
Red bone marrow ceaselessly produces almost all the various types of blood cells required by our body. A rich blood supply guarantees the smooth influx of nutrients and the outflow of mature blood and stromal cells capable of developing into multiple types of cells.Red bone marrow is busy. Our blood cells die constantly. White blood cells, or lymphocytes, usually live for a few hours to a few days; platelets survive for about 10 days; and red blood cells hold out for approximately 120 days.

In adults, red marrow is predominantly located in bones such as the vertebrae, hips, sternum, ribs, and skull and the ends of long bones such as the humerus, femur, and tibia; yellow marrow fills the remaining spongy bone and central cavities of long bones.
Bone Marrow’s Superstars
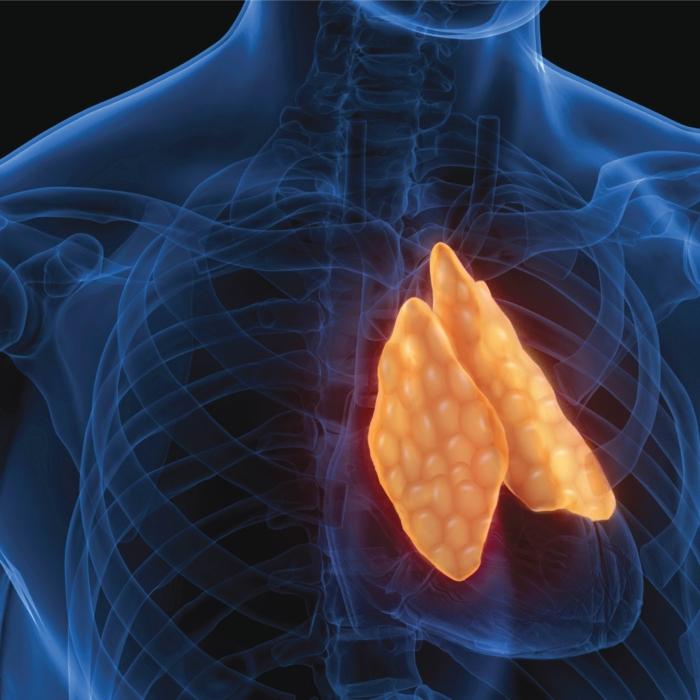
The bone marrow houses stem cells, which possess the ability to turn into two main cell lineages: myeloid and lymphoid.The larger myeloid lineage forms most of the white blood cells (e.g., monocytes, neutrophils, basophils, eosinophils, and dendritic cells), red blood cells, and megakaryocytes, which are the source of platelets.
The smaller lymphoid lineage gives rise to lymphocytes, including T cells, B cells, and natural killer cells—key warriors of the immune system.

Operatives of the Immune System
There are a variety of powerful immune cells released from the bone marrow, including neutrophils, eosinophils, master cells, basophils, monocytes, natural killer cells, and B and T lymphocytes.Cells Derived From the Myeloid Lineage
Neutrophils are the most abundant type of white blood cell and are produced very quickly. They make up about 60 to 70 percent of white blood cells circulating throughout the body. They are the first responders to infections and play a police-like role in innate immunity.
Eosinophils are very effective in fighting against parasites. Parasites are multicellular organisms that immune cells have difficulty swallowing. However, rather than swallowing parasites, eosinophils attack them by releasing chemicals that penetrate their cell membranes. In addition, eosinophils trigger inflammatory reactions in the body by releasing chemicals. They are common factors in allergic reactions. While allergies are often a nuisance, in some cases they have beneficial effects and can protect the body from toxic substances and are linked to lower cancer risk.Macrophages can engulf pathogens in large numbers and are better than neutrophils at attacking pathogens and can do so for longer.
After macrophages and dendritic cells swallow a pathogen, they will analyze it and pass the relevant information to the acquired immune system for further action. They are the “messengers” between the innate and acquired immune systems.
Although their functions are similar, they have their own strengths. Macrophages are stronger in phagocytosis (engulfing and digesting particles), and dendritic cells are better at analyzing and transmitting information, like “signalers.”
Cells Derived From the Lymphoid Lineage
T cells are an important and diverse group of lymphocytes that play a key role in the adaptive immune response. Generally, there are two major types of T cells: helper and cytotoxic. The former aid other immune cells, and the latter kill virally-infected cells and tumors.T cells have many receptors on their surfaces and can bind only to one shape of antigen. An antigen is a substance capable of inducing an immune response found on normal cells in the body and on viruses, bacteria, and tumors.
When a T cell receptor fits with its viral antigen on an infected cell, the cytotoxic T cell will release cytotoxins to kill that cell. Cytotoxic T cells can also kill foreign and cancer cells.
An Unexpected Blood Cell Factory
One might naturally assume that the bone marrow is the sole site that generates blood cells, including the precursors of T and B cells before they mature in the thymus or spleen.However, this is only part of the picture, as emerging research has revealed a mind-boggling array of sometimes unexpected blood makers.
During intestinal transplants, the researchers made an unexpected observation: The transplant recipients began to display the donor’s blood cells in circulation. This phenomenon—blood with two different sets of DNA—is known as blood “chimerism.”
The presence of donor lymphocyte phenotypes indicated the involvement of hematopoietic stem and progenitor cells (HSPCs). Surprisingly, the researchers observed the presence of donor-derived HSPCs within the intestinal mucosa.
It appears that the intestines have a unique ability to produce blood cells.
This was demonstrated when the donor’s blood-generating stem cells were discovered not just in the mucosa of the transplanted intestine, but also in various other parts of the recipient’s body, including the small intestine, liver, and lymph nodes.
The blood cells generated from the transplanted intestines were then distributed to the recipient’s body.

Furthermore, the blood cells derived from the donor tissue appeared to have been educated by the transplant recipient to not attack the recipient’s body; likewise, the recipient’s immune cells were also educated to be tolerant of the donor’s tissues.
This indicates communication between the two sets of blood cells to be friendly with one another. The patients with more donor blood cells had lower organ rejection rates.
Both interesting innovative studies may shed light on a new strategy for managing rejection after organ transplantation.
Gut Bacteria Help Generate Blood Cells
Neutrophils, critical soldiers in the battle against harmful germs in our bodies, have traditionally been understood to be produced in the bone marrow.These findings uncover an interaction between the gut microbiota and the production of granulocytes (the most common type of white blood cell), suggesting a novel way to recover from neutropenia, an abnormally low level of neutrophils.
The gut, once again, proves to be a remarkable source of potential health benefits, including blood generation for the body.
Many people are aware of the fact that 70 percent of our immunity starts in the gut. This is because our gut is the source of nutrition, playing a key role in our immune function. This coincidentally corresponds to the recent studies showing a connection between our gut and the production of neutrophils.
In summary, as one of the most protective organs in the immune system, bone marrow takes the lead in the production of all types of blood cells. However, the marrow is not alone, as it has secret support from the gut and its coexisting bacteria.
◇ References:
Hays K. (1990). Physiology of normal bone marrow. Seminars in oncology nursing, 6(1), 3–8. https://doi.org/10.1016/s0749-2081(05)80127-5.Wang, H., Leng, Y., & Gong, Y. (2018). Bone Marrow Fat and Hematopoiesis. Frontiers in Endocrinology, 9. https://doi.org/10.3389/fendo.2018.00694
Soltan, Muna DDS*; Smiler, Dennis DDS†; Choi, Jennifer H. MBA‡. Bone Marrow: Orchestrated Cells, Cytokines, and Growth Factors for Bone Regeneration. Implant Dentistry 18(2):p 132-141, April 2009. https://pubmed.ncbi.nlm.nih.gov/19359864/
Tahir N, Zahra F. Neutrophilia. [Updated 2023 Jan 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570571/
Kanuru S, Sapra A. Eosinophilia. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560929/
Fong M, Crane JS. Histology, Mast Cells. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499904/
Espinoza VE, Emmady PD. Histology, Monocytes. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557618/
Fu, J., Zuber, J., Martinez, M., Shonts, B., Obradovic, A., Wang, H., Lau, S., Xia, A., Waffarn, E. E., Frangaj, K., Savage, T. M., Simpson, M. T., Yang, S., Guo, X. V., Miron, M., Senda, T., Rogers, K., Rahman, A., Ho, S., . . . Sykes, M. (2019). Human Intestinal Allografts Contain Functional Hematopoietic Stem and Progenitor Cells that Are Maintained by a Circulating Pool. Cell Stem Cell, 24(2), 227-239.e8. https://doi.org/10.1016/j.stem.2018.11.007
Chen, X., Hashimoto, D., Ebata, K., Takahashi, S., Shimizu, Y., Shinozaki, R., Hasegawa, Y., Kikuchi, R., Senjo, H., Yoneda, K., Zhang, Z., Harada, S., Hayase, E., Ara, T., Ohigashi, H., Iwakura, Y., Nakamura, K., Ayabe, T., & Teshima, T. (2022). Reactive granulopoiesis depends on T-cell production of IL-17A and neutropenia-associated alteration of gut microbiota. Proceedings of the National Academy of Sciences, 119(48), e2211230119. https://doi.org/10.1073/pnas.2211230119
Tysoe, O. (2022). New role for bone marrow adipocytes in obesity. Nature Reviews Endocrinology, 18(12), 716. https://doi.org/10.1038/s41574-022-00767-3
Parastoo Boroumand, David C Prescott, Tapas Mukherjee, Philip J Bilan, Michael Wong, Jeff Shen, Ivan Tattoli, Yuhuan Zhou, Angela Li, Tharini Sivasubramaniyam, Nancy Shi, Lucie Y Zhu, Zhi Liu, Clinton Robbins, Dana J Philpott, Stephen E Girardin, Amira Klip (2022) Bone marrow adipocytes drive the development of tissue invasive Ly6Chigh monocytes during obesity eLife 11:e65553. https://doi.org/10.7554/eLife.65553