When to Take Cholesterol Medication
Cholesterol, a waxy substance in the bloodstream, plays a crucial role in transporting fats to various body parts and returning excess fats to the liver for storage. It is also an essential nutrient for cell and hormone production.This may seem paradoxical, as cholesterol is vital for the body, yet high cholesterol levels can increase the risk of heart disease and stroke.
Personally, I do not recommend taking cholesterol-lowering medication but rather advocate using nonpharmacological methods to lower cholesterol. So when is it appropriate to consider cholesterol-lowering medication?
Therefore, it is not necessary to start cholesterol-lowering medication solely based on high blood lipid levels. However, individuals diagnosed with atherosclerosis-induced heart disease, or those at high risk of developing it within the next decade, should consider cholesterol-lowering medication.
Cholesterol Testing
A blood test, typically preceded by an eight-to-12-hour fast, is required to determine cholesterol levels.A blood test measures two types of cholesterol. One is high-density lipoprotein (HDL) cholesterol, which transports excess cholesterol from the blood to the liver, where it is broken down and excreted. The optimal level for HDL cholesterol is 60 mg/dL or higher.
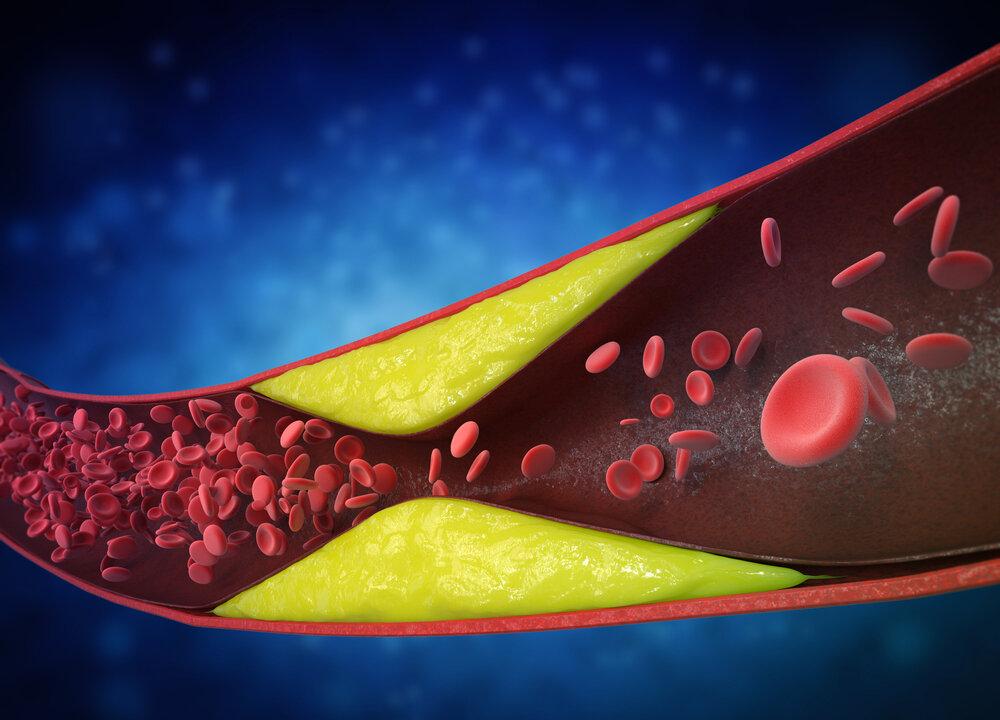
Another type is low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, though this term is not entirely accurate because the body needs both types of cholesterol. LDL cholesterol transports fats to where they are needed in the body; however, elevated levels of LDL can increase plaque accumulation in the arterial walls. For healthy individuals, the optimal level should be below 100 mg/dL.
Role of Statin Medications
There are two sources of cholesterol in the blood: One is produced by the liver, which helps digest fatty foods and produce hormones, and the other comes from the diet, primarily from animal products such as dairy, eggs, meat, and poultry. Reducing dietary cholesterol can help lower blood cholesterol levels. However, some individuals may produce more cholesterol due to genetic factors, and others may absorb more from their digestive systems.A healthy diet, anti-inflammatory measures, and regular exercise are crucial factors in lowering cholesterol. These lifestyle improvements should be made before resorting to cholesterol-lowering medication.
- Low-density lipoprotein (LDL) cholesterol can accumulate in the arteries, and statin medications help reduce LDL cholesterol levels in the blood.
- Plaques are common in most people’s arteries. Statin medications can stabilize these plaques, reducing the likelihood of detachment.
- Statin medications can help regulate cholesterol levels within cell membranes.
- Statin medications also exhibit anti-inflammatory and antioxidant effects.
Side Effects of Statins
Medications, as foreign chemical substances, work by interfering with or even blocking the body’s normal physiological and biochemical processes. Statin medications, for example, work by inhibiting the enzyme in the liver that produces cholesterol. Such inhibition disrupts a normal physiological and biochemical response in the body, potentially leading to side effects.If symptoms are managed solely by medication, it is generally inadvisable to discontinue its use. However, if medication is used as temporary relief while concurrently improving lifestyle, diet, exercise, and stress reduction, it may be possible to gradually reduce or even cease the medication over time. Without lifestyle changes, symptoms are likely to recur after stopping the medication. Medications primarily serve to mask and alleviate symptoms rather than address the underlying causes of the disease.
Comprehensive lifestyle improvements are essential for managing high cholesterol. This includes adopting a healthier diet centered on low-sugar fruits and vegetables, whole grains, legumes, nuts, fish, and poultry, or following a Mediterranean or plant-based diet. Additionally, it is recommended to increase physical activity, avoid smoking, avoid alcohol, and manage weight and diabetes. By making these changes, medication may become unnecessary, or the dosage and duration of medication use can be reduced.
In summary, those with high cholesterol should develop a comprehensive lifestyle change plan based on their personal circumstances rather than relying solely on medication.