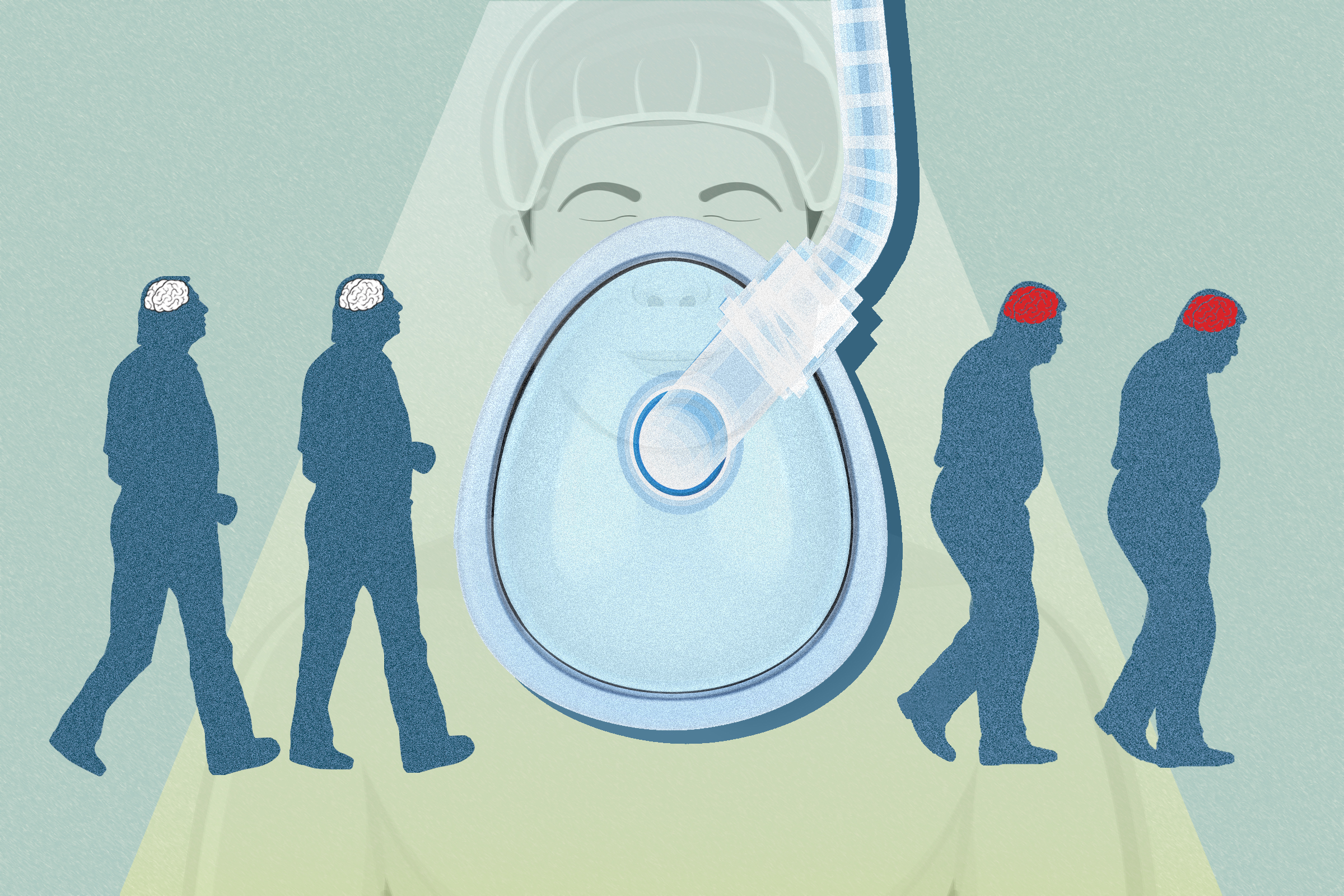
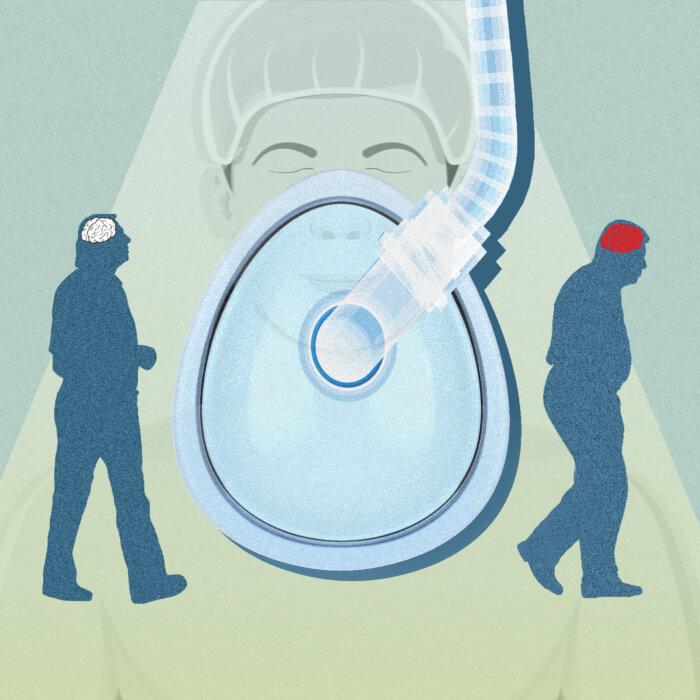
If you’re over 65, there’s a significant risk you will wake up from surgery as a slightly different person. Studies indicate at least a quarter and possibly up to half of this population suffer from postoperative delirium—a serious medical condition that causes sudden changes in thinking and behavior.
It is unclear whether the stress and trauma of surgery are more to blame or the lingering effects of anesthesia, but researchers have found several risk factors that can help identify who is more likely to suffer this condition.
A Growing Concern

Delirium can easily be mistaken for a number of primary psychiatric disorders because its symptoms are also present in conditions such as dementia, depression, and psychosis. Symptoms may also fluctuate by patient and over time.


As awareness of the issue grows, so do concerns over how to protect patients.
Postoperative Delirium Risk Factors
In many cases, those who suffer from delirium after surgery have undiagnosed cognitive impairments prior to surgery. But there are many other known risk factors.Perioperative refers to the time just before, during, and after surgery.

One known cause of delirium is the use of opioids—commonly given for pain reduction during surgery as part of the anesthesia mix and after surgery for lingering pain. The conundrum is that unmanaged high levels of pain during and after surgery also raise the risks for delirium.
Uncontrolled factors such as age and type of surgery also complicate risks. Anyone older than 60, as well as those getting orthopedic or cardiac surgeries—which require longer sedation than elective procedures—are more susceptible, according to the AMA.

What Does Delirium Have to Do With Anesthesia?
Delirium is more common among patients who are using multiple medications. Surgeries almost always involve anesthesia drugs on top of medications that may be given for pain, as well as precautionary antibiotics. A variety of studies have attempted to understand the role of anesthesia.“It’s not something to be taken lightly. The risks can be severe because of all the organ systems we are encountering,” Dr. Matt Hatch, anesthesiologist and vice chair of the American Society of Anesthesiologists’s committee on communication, told The Epoch Times.
Anesthetic drugs have been proven safe for what they do: keeping patients alive but unaware during surgery. Yet there are inherent risks that are complicated by the frailty of the human mind and medical status, among other factors.

“Trying to minimize risks of the anesthesia on the elderly brain is something I worry about, especially as I take care of elderly patients in their mid-to-late 80s, 90s, and even to 100 every once in a while,” Dr. Hatch said.
Larger studies with longer follow-ups suggest that there is an inherent risk of postoperative delirium when general anesthesia is used, though some smaller studies with shorter follow-up times don’t find an association.
Conflicting findings in other studies suggest that perhaps it is the amount of sedation or type that may have an impact.


The Risk of Going Under
A person’s tolerance to surgery has a lot to do with their reserve, explained Dr. Kaveh, who has the unique perspective of being a Stanford and Harvard-trained anesthesiologist and integrative medicine specialist. He explained reserve as “extra bandwidth” to withstand fluctuations in blood flow, tissue damage, and other trauma.Nutrition, physical fitness, and positive psychosocial traits can improve reserve. However, unlike cardiac reserve, which can be tested, Dr. Kaveh said cognitive reserve is more complicated to assess. That means that it can be difficult to fully determine a patient’s risk of delirium after anesthesia.
While some may think anesthesia is simply putting someone asleep, it is far more impactful.
“We are literally turning off light bulbs in the brain and central nervous system. It’s not just sleep,” Dr. Kaveh said. “If you put electrodes on the head, it’s not the same electroencephalogram, EEG, signature you see when people are sleeping. It’s more like a coma.”

Anesthesiologists rely on a presurgical exam—at least in non-emergency situations—that might more closely resemble the first appointment with a new primary care provider. An anesthesiologist needs to know a full history of medications, supplements, physical condition, previous surgeries, diagnoses, diet, physical activity, drug use, and perhaps most importantly, anxiety in general and related to the procedure.
All of this determines the various types and doses of anesthesia drugs used during the procedure—a combination of gasses and drugs that can lower pain, keep the body in a comatose state, reduce postoperative delirium, and even induce temporary amnesia.
No two patients get the same anesthesia cocktail, making it a personalized approach that depends on a number of variables.

“We have to operate on a spectrum. It’s why we go to school for so many years so we know the safe amounts to administer and how to resuscitate the body based on where it is on the scale to keep it functioning so it wakes up at the end of surgery,” Dr. Kaveh said.
The reality is that patients who aren’t in optimal psychological health face more risks of complications. That’s often because they’re more likely to take prescribed or illicit drugs—marijuana is the most common one—to cope with anxiety, and it can increase their anesthesia needs, Dr. Kaveh said.
Taking Steps to Protect Your Brain

The Global Council on Brain Health report spells out dozens of things that patients and their caregivers can do to lower risks, including being honest about their anxiety levels.
Dr. Hatch said patients who adopt a positive mindset and use visualization techniques can lower their need for pharmaceuticals. This can include the amount of anesthesia required.
Other helpful ideas include bringing familiar items from home such as hearing aids, glasses, dentures, and all medications and supplements. It’s also important to eat well, get exposure to sunlight, prioritize sleep, and get back to a regular routine as soon as possible.

More experts and surgeons are also recognizing the importance of post-surgical cognitive rehabilitation. Just as patients who are having orthopedic and other surgeries are guided to get up and move shortly after surgery, there’s evidence that doing crossword puzzles and other cognitive-based activities can help prevent delirium, Dr. Hatch said.
“Most of these things don’t require risk, much cost, or even medications,” Dr. Kaveh said. “This is just establishing humanity and treating people with dignity. If we can do that for patients after surgery, especially those at risk, and their family can advocate, we can lower a lot of the emotional toll surgery takes on people.”
In fact, sleep and a support system appear to be two vital ways to prevent delirium. Hospital staff routinely wake sleeping patients for medication, and the various beeps of hospital equipment can disrupt sleep. For those who are hospitalized after surgery, minimizing sleep disruptions is key, according to the Anesthesia & Analgesia article.
“This is particularly important for the older patient for whom the restorative properties of natural sleep are another key part of their recovery. Importantly, family engagement and social support should be implemented early in the preoperative period,” the article states.
Detoxing the Drugs
Rosia Parrish, a naturopathic doctor, said the inherent risks and side effects of anesthesia can be offset by boosting the body’s antioxidant capacities both before and after surgery.“It depletes glutathione, a vital antioxidant that protects cells from oxidative stress. Reduced glutathione levels may hinder the body’s healing ability after surgery,” Ms. Parrish told The Epoch Times in an email.
Glutathione depletion weakens the immune system, she said, and causes muscle weakness and pain, joint discomfort, and cognitive issues including brain fog, difficulty concentrating, and memory problems. It also causes fatigue and low energy due to cellular damage, as well as worsening mood problems because of its role in neurotransmitter regulation, leading to anxiety and depression.
She offered many recommendations to facilitate the body’s detoxification process after anesthesia, including supplements such as milk thistle, N-acetyl cysteine, curcumin, glutathione, vitamin C, dandelion root, chlorella, spirulina, burdock root, nettle, cilantro, ginger, and green tea.



Dr. Kaveh said the best way to detox from the drugs is to be healthy in the first place so that you won’t require larger doses of medications.
Be sure to talk with your doctor or anesthesiologist about supplements that you plan to take, as some can interact with medications, Dr. Hatch said. He said there’s really no need to detox after surgery, especially for those who don’t have kidney and liver problems, which may slow the process of drug removal from the body.
Additional Reading: Details of Delirium
Based on evidence and research to date, the Global Council on Brain Health laid out known facts about delirium, including the following:- Delirium can come and go and manifest in very different ways in hours or days.
- Delirium may last a few days, weeks, or remain permanently.
- Delirium is most common in health care settings after an injury, illness, surgery, dehydration, infection, or change in medication.
- Delirium is often overlooked, misdiagnosed, or improperly managed.
- Many health care providers are unaware of delirium.
- Delirium may be a sign of other health problems.
- Delirium can lead to falls, prolonged hospital stays, and a loss of independent living.
- Hearing or vision problems, frailty, underlying medical conditions, alcohol or drug abuse, and opioid use are risk factors for delirium.