A new study has linked psychedelic use that results in emergency room (ER) visits with an increased risk of schizophrenia.
The research, published on Nov. 13 in JAMA Psychiatry, found that people who went to the ER for hallucinogen-related issues were more than 21 times more likely to be diagnosed with schizophrenia spectrum disorders (SSDs) within three years compared to the general population.
The study tracked more than 9 million people.
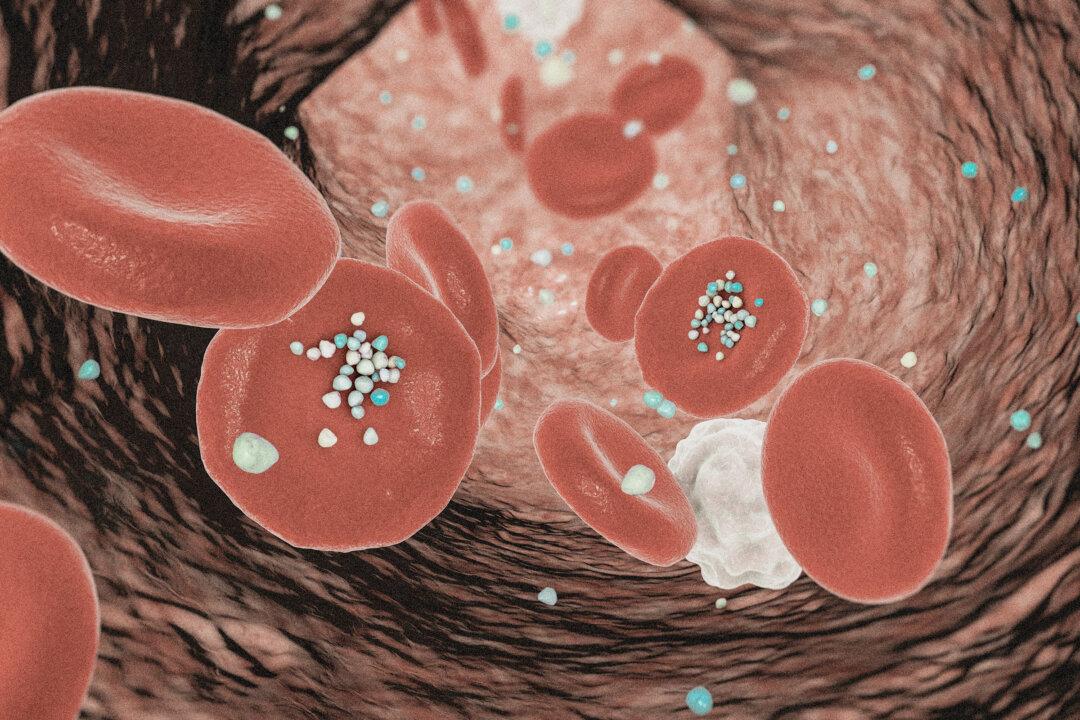
The findings come as psychedelics—such as psilocybin (magic mushrooms), LSD (acid), DMT (ayahuasca), and MDMA (ecstasy)—are becoming more popular, both recreationally and in therapeutic settings to treat some mental health conditions.
Psychedelics, or hallucinogens, are substances that change the way one sees, feels, and experiences the world, often causing hallucinations and altered perceptions.
“Our study examines the risk associated with having an ER visit involving hallucinogen use, not hallucinogen use itself,” Dr. Daniel Myran, research chair in social accountability at the University of Ottawa, told The Epoch Times in an email, noting that the findings do not establish a direct causal relationship between hallucinogen use and schizophrenia.
“To me, the findings highlight how little we know about the long-term mental health risks of hallucinogen use,” he stated.
Hallucinogens Linked to Psychosis Risk
The study found an increase in ER visits for hallucinogen use in recent years—with visits rising by 86.4 percent between 2013 and 2021, after remaining stable from 2008 to 2012.“This trend mirrors the rise in hallucinogen use in the U.S., which has more than doubled in individuals aged 19 to 30 over the past eight years,” Myran wrote.
The study also found that hallucinogen use—particularly when it leads to psychosis—is strongly linked to an increased risk of SSDs, which include schizophrenia, delusional disorder, and brief psychotic disorder.
Among those who experienced psychosis after using hallucinogens, the risk of developing schizophrenia or related disorders within just three years was nearly 15 times greater than in the general population.
The research tracked more than 9.2 million individuals and analyzed ER visits related to hallucinogen use from 2008 to 2021. Among this population, more than 5,200 sought ER care for issues such as harmful use, intoxication, dependence, and hallucinogen-induced psychosis.
Hallucinogens Versus Alcohol and Cannabis
The study also examined the relationship between alcohol and cannabis use and SSD diagnosis. It found that ER visits related to hallucinogen use were associated with a risk of SSDs that was five times higher than the risk of SSDs for alcohol-related visits and 1.5 times higher than the risk for the group that made cannabis-related ER visits.Although this research does not establish a causal relationship between hallucinogen use and schizophrenia, the authors stressed that the findings highlight significant risks, particularly for those with a predisposition to psychosis or schizophrenia.
The Role Hallucinogens Play in Schizophrenia
A psychotic episode doesn’t mean someone will develop schizophrenia, but it does signal an increased risk, Dr. Jacob Ballon, an associate professor of psychiatry and behavioral sciences at Stanford Medicine who was not involved in the study, told The Epoch Times.While both hallucinogens and schizophrenia involve hallucinations and altered perceptions of reality, the two experiences are not identical, according to Ballon, who specializes in the treatment of people with psychotic disorders, including schizophrenia.
Hallucinations caused by psychedelic drugs, such as LSD or psilocybin mushrooms, are typically temporary and less intense than those seen in schizophrenia. However, for people with a predisposition to psychosis, hallucinogen use may trigger underlying symptoms.
People at high risk for schizophrenia—those showing early signs of mental illness but who are not yet diagnosed—may use hallucinogens as a way to cope with anxiety or depression, Ballon added. Hallucinogens can act as a trigger for people in this high-risk state, he said. They may bring latent psychosis to the surface, potentially leading to the onset of schizophrenia.
Hallucinogens affect different brain systems than stimulants such as amphetamines that are often used to treat conditions such as attention-deficit/hyperactivity disorder (ADHD), which is closely linked to schizophrenia, Ballon stated.
While it is not uncommon for amphetamines to “unmask a psychosis,” as they act on the dopamine-related pathway often related to schizophrenia, hallucinogens do not.
Implications for Therapeutic Uses
There has been increasing academic and clinical interest in the use of psychedelics for mental health treatment.Ballon drew a parallel to cannabis, noting how the more potent strains available today differ from the milder varieties of the past. He suggested the trend of increased use and potency of hallucinogens could make them more dangerous, especially for those vulnerable to psychosis.
Early Intervention
Recognizing early signs of psychosis and intervening promptly is essential, particularly for those at risk of developing schizophrenia.The onset of schizophrenia is often preceded by subtle, “attenuated” symptoms, such as hearing voices or holding unusual beliefs, yet maintaining some insight into their abnormality, according to Ballon. He noted that family members should be concerned if someone begins withdrawing socially or experiences significant behavioral changes.
For those who experience a psychotic episode after using hallucinogens, Ballon recommends monitoring for signs of worsening mental health, such as increased social withdrawal, sleep disturbances, or a decline in daily functioning.
The sooner people at risk seek help, the better their chances of minimizing long-term mental health challenges, Ballon said.