Researchers at the University of Helsinki observed that the presence of these bacterial strains in Parkinson’s patients could lead to the aggregation of alpha-synuclein, a protein closely associated with the disease.
To further investigate this association in humans, the researchers analyzed stool samples from 10 Parkinson’s patients and 10 healthy individuals. The findings show that all Parkinson’s patients had Desulfovibrio bacteria in their gut microbiome, establishing the link between these bacteria and the disease.
Gut May Be Where Parkinson’s Disease Starts
“The cause of Parkinson’s disease has gone unknown despite attempts to identify it throughout the last two centuries,” Per Saris, professor of microbiology at the University of Helsinki and study co-author, said in a statement.“Our findings are significant," Saris said.
They suggest that certain strains of Desulfovibrio bacteria are highly likely to be a causative factor in Parkinson’s. He also noted that environmental factors are the primary cause of the condition.
The study discovered that Desulfovibrio strains obtained from individuals without Parkinson’s disease didn’t induce alpha-synuclein aggregation to the same extent.
Desulfovibrio bacteria produce hydrogen sulfide as a result of their metabolic processes.
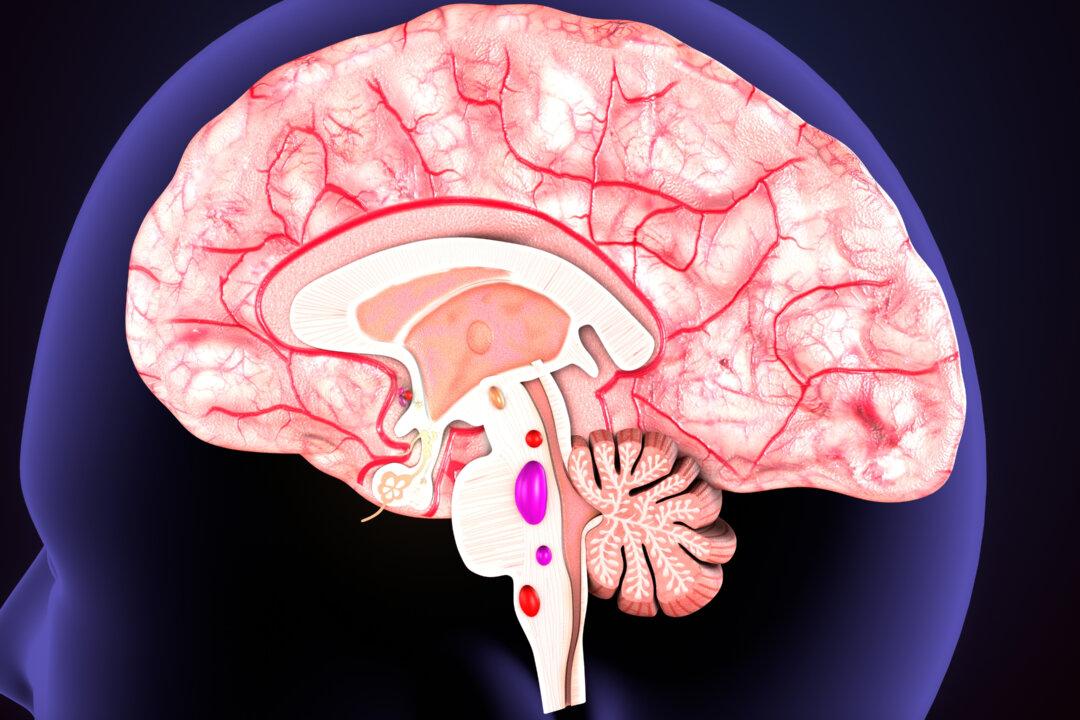
Hydrogen sulfide is a gas neurotransmitter and can play an important role in the development of Parkinson’s, Dr. Mary Kay Ross, a fellow of the American College of Emergency Physicians and founder of the Brain Health & Research Institute, told The Epoch Times.
“Hydrogen sulfide can also raise the iron content in the cytoplasm, which exacerbates that alpha-synuclein aggregation,” Ross said.
The excessive presence of Lactobacillus, a probiotic, and the imbalance of various other bacteria also play a role in Parkinson’s patients, Dr. Guy Schwartz, co-director of the Stony Brook Parkinson’s and Movement Disorders Center at Stony Brook Medicine, told The Epoch Times.
“That’s a deviation from the normal, healthy, non-Parkinson’s disease colonization of the colon,” Schwartz said.
Similar patterns are also seen in diseases such as autism and irritable bowel syndrome.
Constipation, Parkinson’s, and the Gut
The abundant bacteria may produce harmful substances or hinder the growth of beneficial bacteria that may play a role in preventing Parkinson’s disease, Schwartz said.“Intestinal motility is also decreased with the high levels of hydrogen sulfide, which leads to constipation, seen in Parkinson’s; increased inflammation; and enhanced central nervous system damage,” Ross said.
Constipation exacerbates the problem.
“The fecal matter doesn’t flow at a normal rate, in a normal volume, and this causes backup, and this backup is into the small intestine, and bacteria don’t belong in the small intestines,” Schwartz said.
This leads to colonies of bacteria from the colon accumulating in the small intestine.
Treatments for Patients With Abnormal Microbiome
“My Parkinson’s patients seem to always have very abnormal microbiomes,” Ross said.“We have tried to treat these patients using a blend of prebiotic fibers to feed the desired bacteria and change the microbial environment, but the Parkinson’s patients have only gotten worse, and then better once we stopped the prebiotics,” Ross said.
There was concern regarding the possibility of bacteria metabolizing drugs such as dopamine, potentially exacerbating the symptoms, according to Ross.
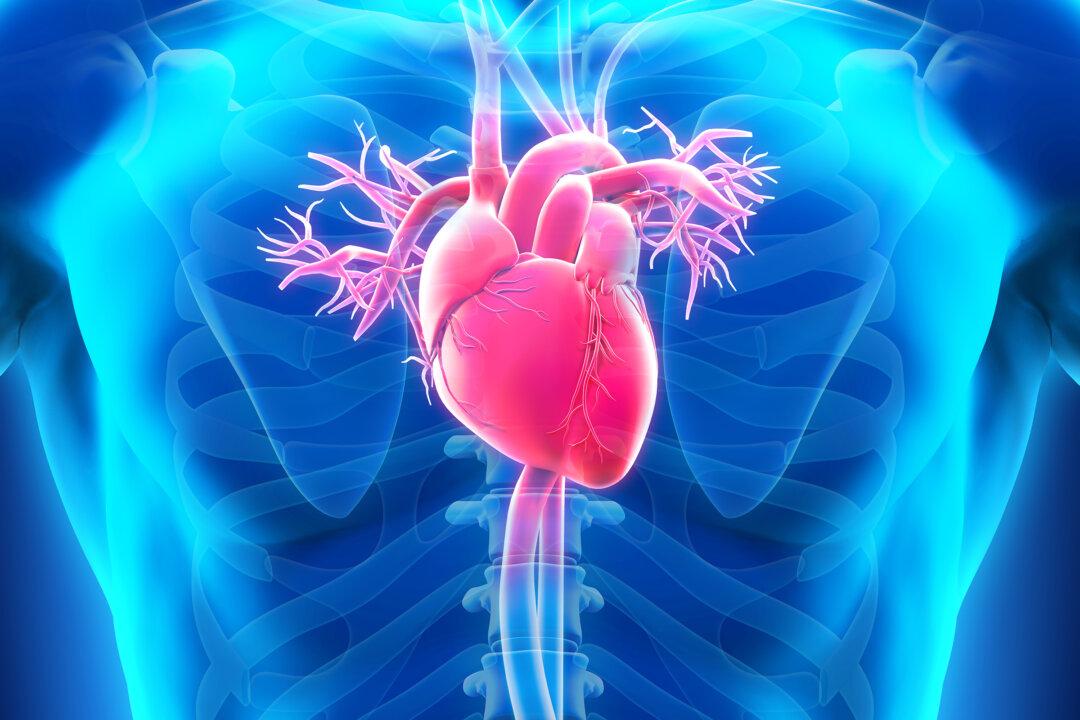
The Possible Role of the Gut-Brain Connection in Parkinson’s
Studies have shed light on the intriguing link between the gut microbiome and Parkinson’s disease, suggesting a potential role of the gut-brain axis in the development and progression of the condition.The feeling of “butterflies” in our gut is linked to our nervous system, Ross explained, highlighting that this is a genuine phenomenon and an indicator of the functioning of the gut-brain axis.
“The gut-brain axis is a bidirectional communication system between the gastrointestinal tract, the gut, and the central nervous system—the brain,” she said.
“There is a great deal of emerging research that suggests that alterations in the microbiome or the gut-brain axis can impact neurodegenerative diseases through several different mechanisms.”
Understanding the influence of the gut-brain axis on neurodegenerative diseases opens up novel opportunities for therapeutic interventions. These approaches may involve dietary modifications, the use of probiotics, and fecal microbiota transplantation to target the microbiome.
“However, further research is needed to fully comprehend the intricate mechanisms involved and develop effective interventions,” Ross said.