What Are the Symptoms and Early Signs of Lyme Disease?

- Fever.
- Chills.
- Headache.
- Sensitivity to light.
- Fatigue.
- Muscle aches.
- Swollen lymph nodes.
- An erythema migrans (EM) rash that may appear in a “bullseye” shape. Contrary to popular belief, the bullseye is not as typical as other manifestations of the rash. It is more typically uniform in color, round (like a spider bite), and/or bluish in color.
- More severe headaches.
- Facial palsy (nerve weakness on one side of the face).
- Arthritis.
- Pain in the bones.
- Heart palpitations or an irregular heartbeat.
- Dizziness.
- Nerve pain.
- Inflammation in the brain or spinal cord.
- Numbness in the hands or feet.
What Causes Lyme Disease?
For an infection to occur, a tick typically must be attached to a person’s skin for 36 to 48 hours before bacteria begin to be transmitted. If ticks are found before this window of time, there is a chance that Lyme disease transmission can be avoided.

What Are the Stages of Lyme Disease?
- Stage 1 (early localized): Lyme disease is localized. Patients may present with a rash, known as erythema migrans, on or near the bite site and/or with a low-grade fever. This initial stage typically occurs within the first month following a tick bite. Many people may not exhibit any signs or symptoms in stage 1.
- Stage 2 (early disseminated): People may experience more symptoms in this stage, including fatigue, dizziness, and cardiac-based symptoms. Stage 2 Lyme disease typically develops between weeks three and 12 after an infection. This is the stage in which Lyme disease is more disseminated, or has spread, throughout the body.
- Stage 3 (late persistent): This stage typically develops months to years after an infection. During this stage, neurological symptoms, arthritis (especially in the knees), and heart rhythm complications may be common. It is vital to seek medical treatment if experiencing these symptoms.
- Babesia: This malaria-like parasite infects red blood cells and may induce similar symptoms to Lyme disease. This is typically treated with antimalarial drugs and antibiotics.
- Bartonella: These bacteria infect red blood cells and may induce a streaked rash similar to stretch marks. Bartonella also must be treated with a combination of antibiotics.
- Rickettsia: These bacteria can cause fever, severe headache, rash, and muscle pain and weaken the body’s blood vessels. The condition is typically treated with oral medications and/or intravenous antibiotics. The most common rickettsial infection in the United States is Rocky Mountain spotted fever.
Who Is at Risk of Lyme Disease?
Because Lyme disease is preventable, one must be aware of the risk factors that put an individual at a higher risk for developing it.
Most of the time, people have a higher risk of being infected during the spring through fall, but it’s possible to be infected if the weather stays above freezing.
- Living in certain states and regions in the United States, including the Northeast, mid-Atlantic states, Wisconsin, Minnesota, and northern California.
- Living in suburban or more rural areas, as areas with more vegetation increase one’s likelihood of encountering ticks.
- Working outside.
- Outdoor activities like hiking, hunting, or gardening in higher transmission areas.
- Having pets that may bring ticks in from outside.
How Is Lyme Disease Diagnosed?
- Blood tests: Diagnosing Lyme disease usually is a two-step process. Blood tests look for bacteria buildup in the body that causes Lyme disease. The first recommended blood test is an enzyme-linked immunoassay (ELISA) test that tests for antibodies in your blood formed to fight Lyme disease. It can return with false negatives if performed too close to the time of the suspected bite, as it takes a few weeks for the antibodies to develop. Two options are available if a second test is needed: a second ELISA test or a Western blot, which is sometimes preferred for later-stage Lyme disease.
- Cerebrospinal fluid (CSF) test: A CSF test may be performed if Lyme disease has been thought to affect your nervous system and/or if blood test results come back inconclusive.
- Polymerase chain reaction (PCR) tests: PCR tests can detect the genetic material (DNA) of the Lyme bacteria. These tests are typically only accurate if a person has an active infection.
What Are the Complications of Lyme Disease?
- Persistent fatigue.
- Inflammation and arthritis: A person may experience joint pain and/or swelling in the knees, elbows, shoulders, wrists, ankles, or hips. This can usually be treated with antibiotics and/or nonsteroidal anti-inflammatory drugs (NSAIDs).
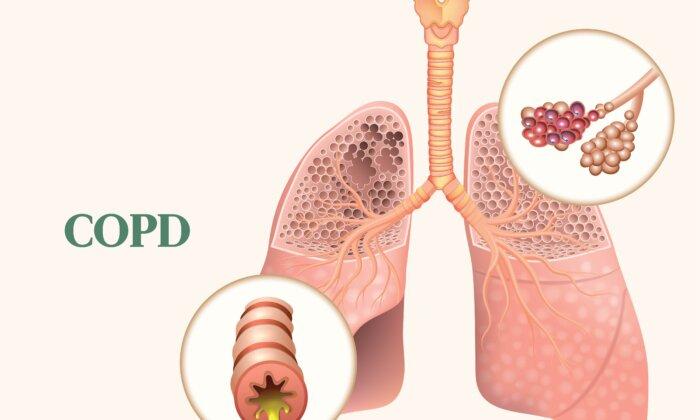
- Nerve damage: Nerve damage may result in weakness in several areas of the body and may also cause pain, numbness, and/or tingling.
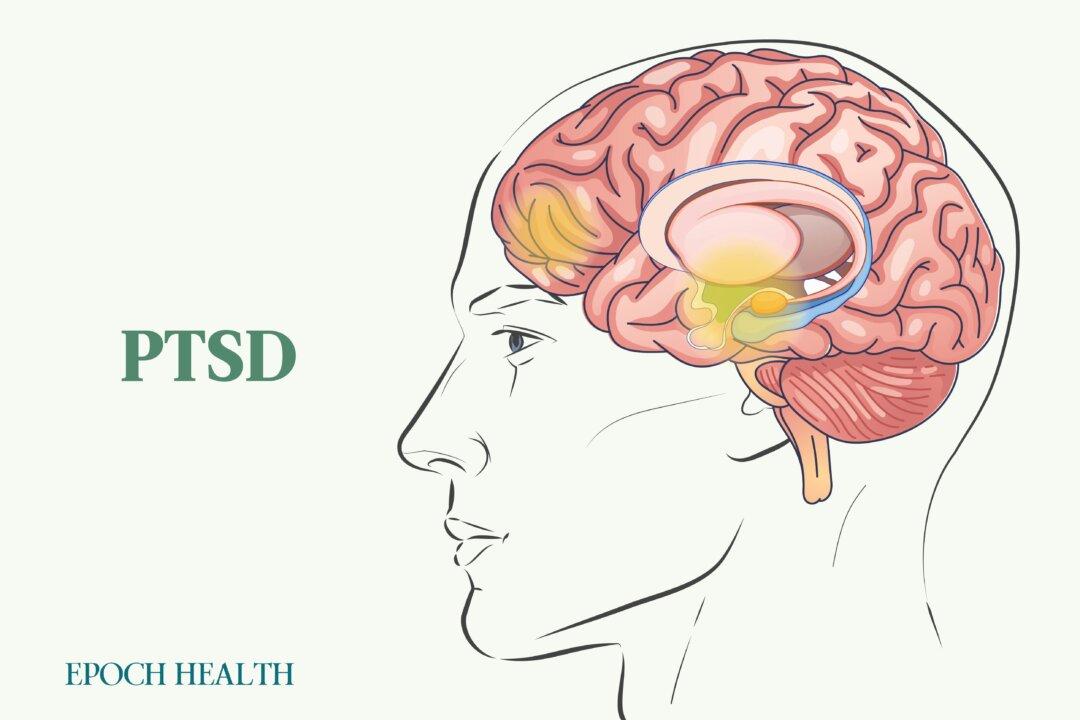
- Neurological complications: Neurological complications, also known as neuroborreliosis, like confusion, loss of memory, difficulty concentrating, or other speech problems are possible.
- Post-Lyme disease syndrome: This condition can occur after Lyme disease has been treated with antibiotics. If this happens, people may experience persistent fatigue, aching muscles, trouble with cognition, and headaches. This syndrome is often diagnosed if people are still experiencing symptoms six months post-treatment.
- Lyme carditis: This rare but serious complication occurs in about 1 percent of cases.
What Are the Treatments for Lyme Disease?
Antibiotics
Oral antibiotics such as doxycycline, amoxicillin, and cefuroxime are used to help fight Lyme disease. Additional medication may be prescribed to manage Lyme disease symptoms, such as those that target pain, inflammation, or cognition.What Unique Problems Do Those Living With Lyme Disease Face?
Lyme disease—especially in its later stage—can be very difficult to treat, and the symptoms debilitating. The bacteria that cause it can evolve and adapt to treatment methods, namely antibiotics. For this reason, attempting to treat Lyme disease with both antibiotic and holistic remedies is often recommended. As with any chronic illness, helping individuals bolster their immune systems to aid in reducing symptoms and fighting the illness is paramount.
How Does Mindset Affect Lyme Disease?
What’s promising is that some research indicates that positive mental health practices can significantly improve perceived quality of life and symptom recurrence for those with Lyme disease.
To begin, it is helpful to monitor symptoms and perceived quality of life by keeping a symptom journal to share with a health care provider. This can help begin to track symptom recurrence and identify patterns. Monitoring things like changes in appetite, energy, and mood are all helpful indicators of overall mental health status that can give a health care provider more insight into how to provide personalized guidance and suggestions.
What Are the Natural Approaches to Lyme Disease?
- Bandit.
- Oregano.
- Clove bud.
- Geranium bourbon.
- Cinnamon bark.
Because the majority of the immune system resides in the gut, and the gut is where nutrients are absorbed, the health of your microbiome is vital. Including anti-inflammatory, fiber-rich foods can help feed the good gut bacteria within the gastrointestinal system and thus improve overall immunity. Including foods like fatty fish, vegetables, healthy fats, fruits, and whole grains is a great jumping-off point for building an anti-inflammatory regimen. For personalized guidance, it is always advised to consult a qualified health care provider.
- Stress-reducing techniques to help manage pain (therapy, meditation, etc.).
- Mind-body practices like qigong to help improve posture, movement, and breathing techniques.
- Acupuncture to aid in reducing fatigue.
- Cognitive behavioral therapy (CBT) and relaxation techniques to help promote a better night’s sleep.
- Lemon balm and/or melatonin supplements to aid in sleep.
- Online brain training exercises to aid in enhancing concentration and/or working memory for those experiencing cognitive symptoms.
How Can I Prevent Lyme Disease?
- Remaining aware of environmental exposure: In areas with tall grass or overgrown brush, wear long pants and sleeves to mitigate exposure. In addition, staying in the middle of trails while hiking, wearing insect repellent, and showering immediately after returning from an outdoor activity can help. Also, tuck pant legs into socks when walking through tall grass.
- Self-examination: If you think there is a chance that you or a family member could be exposed to ticks, it is advised to do self-examinations each time you come back from an outdoor activity. If you find a tick, it is important to properly remove it immediately, ensuring you pluck it by the head and not by its exposed backside.
- Creating a tick-free zone: Creating a tick-safe zone is advised if you live or work in a high-risk area. Using chemical control agents and keeping deer away are helpful tips for reducing risk.