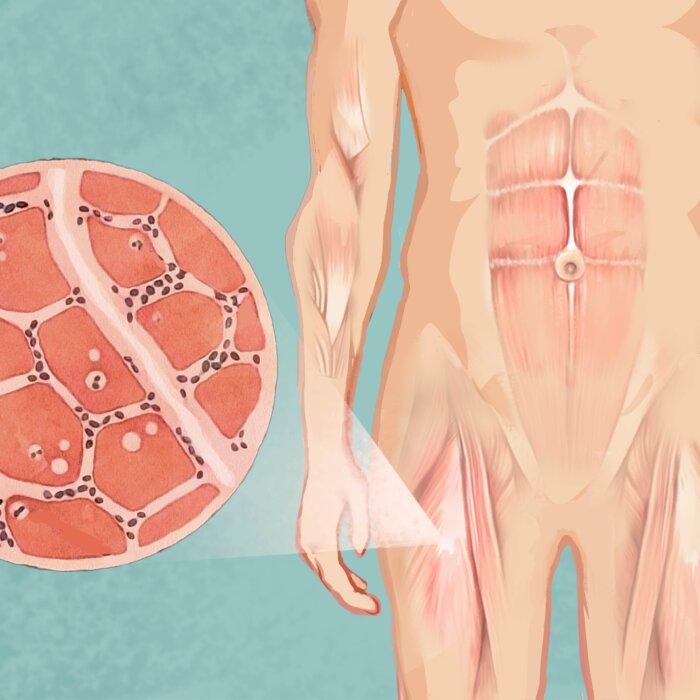
Sarcopenia is a musculoskeletal condition characterized by the age-related loss of muscle mass, strength, and function. Although less commonly seen in some infants and children, regular muscle loss typically begins in a person’s 30s or 40s (though sometimes later) as skeletal muscle mass gradually shrinks (atrophy). By their 70s, people may retain only around half the muscle mass they had in their 20s.

What Are the Symptoms and Early Signs of Sarcopenia?
- Reduced muscle size
- Muscle weakness or reduced strength
- Reduced stamina
- Impaired balance
- Difficulty climbing stairs
- Slower walking speed
- Difficulty performing daily tasks
- General weakness
What Causes Sarcopenia?
1. Hormone Imbalance
An age-related reduction in hormones such as testosterone, thyroid hormone, and insulin-like growth factor contributes to muscle loss and weakness. These hormonal changes and increased pro-inflammatory cytokines promote muscle breakdown and hinder muscle maintenance.2. Decreased Protein Synthesis and Regeneration
Sarcopenia is influenced by a decline in muscle protein synthesis (creation), which is essential for maintaining muscle mass. As people age, the balance between protein breakdown and synthesis shifts, with synthesis rates declining. Less synthesis leads to muscle loss. Muscle’s ability to regenerate after injury or stress also declines with age, partly due to decreased satellite cells, which are essential for muscle tissue repair and growth.3. Motor Unit Remodeling
Over time, the number of motor neurons (cells that aid in movement) in the spinal cord declines. Motor units, which are motor neurons and their associated muscle fibers, also decrease. This irreversible process results in a progressive loss of muscle mass and strength.As we age, the body undergoes motor unit remodeling, where the nerve supply to muscles shifts via denervation and reinnervation. Remodeled motor units may be less efficient, resulting in slower movement and muscle weakness.
What Are the Types of Sarcopenia?
1. Primary
Also known as age-related sarcopenia, primary sarcopenia is diagnosed when no other specific cause for muscle loss can be identified. It is linked to issues such as mitochondrial dysfunction, reduced muscle repair capacity, nerve and muscle communication problems, reduced production or sensitivity to muscle-building hormones, and age-related appetite loss.2. Secondary
Secondary sarcopenia occurs when factors other than aging, such as systemic diseases like cancer or organ failure, contribute to muscle loss. There are also several subtypes of secondary sarcopenia, including:- Activity-related sarcopenia: This subtype is caused by a sedentary lifestyle, prolonged bed rest, lack of physical activity, deconditioning (reduced physical abilities due to lack of activity), or zero-gravity conditions.
- Disease-related sarcopenia: This is associated with chronic diseases such as cancer, kidney disease, advanced organ failure (e.g., brain, kidney, or lung failure), or chronic obstructive pulmonary disease (COPD).
- Nutrition-related sarcopenia: This is linked to malnutrition, inadequate protein intake, or nutrient malabsorption.
Who Is at Risk of Sarcopenia?
- Age: Individuals aged 40 and older are at a higher risk.
- Inactivity: Lack of exercise is considered the primary risk factor for sarcopenia. Muscle cell numbers gradually decline around age 50, with the loss of muscle mass and strength being more pronounced in sedentary individuals than physically active individuals.
- Medical conditions: Sarcopenia is highly common in individuals with cardiovascular disease, dementia, diabetes, and respiratory conditions. Some research also suggests a potential link between sarcopenia and rheumatoid arthritis. Some of these diseases may directly harm the muscles, while others can make people less physically active or eat less due to loss of appetite.
- Malnutrition: Nutrition is a key modifiable risk factor for older adults, who often eat less and are at risk of malnutrition. Insufficient protein intake is common and can adversely affect muscle mass and overall health. In addition, impaired nutrient absorption may also lead to nutrition-related sarcopenia.
- Obesity and insulin resistance: As people age, some may develop a condition called sarcopenic obesity, where they gain fat while losing muscle. This can lead to insulin resistance (improper response to insulin). Insulin resistance causes more fat to build up around the organs and makes it harder for muscles to grow or avoid breaking down. At the same time, having less muscle means the body doesn’t use sugar as effectively, which can worsen insulin resistance.
- COVID-19 infection: A 2021 study found that severe inflammation inflicted by COVID-19 worsens aging-related immune decline, damages blood vessels, and disrupts cell function, leading to muscle breakdown and acute sarcopenia.
- Smoking: A 2021 study found that smokers face a 2.36 times higher risk of developing sarcopenia. Additionally, they have a 2.68 times greater likelihood of developing severe sarcopenia compared to nonsmokers. Also, for each additional cigarette smoked per day, the risk of developing sarcopenia increased.
- Space travel: Astronauts or people who travel in space are more at risk of sarcopenia.
How Is Sarcopenia Diagnosed?
- Low muscle mass (mandatory criterion)
- Reduced muscle strength
- Low physical performance
- Mild: only low muscle mass
- Moderate: low muscle mass and either reduced muscle strength or low physical performance
- Severe: all three criteria present
Find
The “strength, assistance with walking, rising from a chair, climbing stairs, and falls” (SARC-F) questionnaire assesses self-reported difficulties with the described tasks. The answer to each question is scored between zero and 2, with a maximum score of 10. Research suggests a score of 4 or higher indicates the need for further, more detailed evaluation.A hand test and chair test may be performed to test muscle strength.
The handgrip test assesses overall muscle strength, as handgrip strength correlates with strength in other muscles. The recommended cutoff for handgrip strength is <27 kilograms for males and <16 kilograms for females.
Assess and Confirm
There is no consensus on the best method for confirming sarcopenia. However, some of the tests a health care provider may perform include:- MRI: MRI is considered the “gold standard” for confirming sarcopenia, as it provides highly accurate measurements of total body muscle mass.
- Computed tomography (CT): CT is also considered a “gold standard.”
- Dual-energy X-ray absorptiometry (DEXA): DEXA (or DXA) uses low-energy X-rays to measure skeletal mass. Although less accurate than CT or MRI, DEXA is more convenient, making it a widely available and practical option for assessing sarcopenia.
- Bioelectrical impedance analysis (BIA): BIA can measure body composition, particularly muscle mass, fat mass, and total body water. It works by sending a low, safe electrical current through the body and measuring the resistance (impedance) to the flow of electricity. It is likely the most accessible and portable method for quantifying muscle mass. BIA scales (aka body fat scales) are widely available for purchase.
Severity
The measurement of physical performance determines sarcopenia severity. The EWGSOP2 recommends the following tests and cutoff points to assess severity:- Gait speed test: The gait speed test is simple and practical. The “4-meter usual walking speed test” measures the time it takes for a patient to walk 4 meters at their normal pace. It helps predict adverse effects linked to sarcopenia.
- Short physical performance battery (SPPB): The SPPB consists of three timed tasks: the chair stand test, standing balance, and walking speed.
- Timed up and go (TUG) test: The TUG test measures the time it takes for a patient to stand up from a chair, walk 3 meters away and back, and then sit down again.
- 400-meter walk test: This test involves a patient walking 20-meter laps at a comfortable pace and achieving 400 meters, with a maximum of 2 minutes of rest between each lap.
What Are the Possible Complications of Sarcopenia?
- Increased risk of falls, fractures, cognitive impairment, metabolic disorders, and hospital-acquired infections.
- Extended duration and necessity of hospitalizations.
- Increased risk of mortality in patients with end-stage kidney disease, pancreatic cancer, and chronic heart failure. It is also associated with increased mortality in patients having general or colorectal surgery.
- Increased risk of dose-limiting toxicities (DLT): Sarcopenia is linked to increased DLT (when the side effects of medications become intolerable or dangerous) in patients receiving chemotherapy for renal cell carcinoma, hepatocellular carcinoma, and breast cancer.
- Increased risk of postoperative complications: Sarcopenia is linked to a higher risk of postoperative complications in patients undergoing general surgery and liver transplant.
What Are the Treatments for Sarcopenia?
1. Physical Activity
Physical activity helps reduce muscle loss and enhance strength in sarcopenia, serving as an effective strategy for both prevention and management. An exercise regimen is regarded as fundamental in the treatment of sarcopenia. Exercise routines that incorporate several exercise types may be more effective than those focusing on just one type of exercise.- Strength training: Strength (resistance) training should be prioritized as a primary treatment and prevention strategy for sarcopenia. Weights, resistance bands, exercise machines, or body weight can be used. As they age, people who don’t engage in strength training can lose 4 to 6 pounds of muscle per decade, often replaced by fat. Exercises may include standing calf raises, chair stands, reverse fly, and overhead press.
- Aerobic exercise: Aerobic exercise helps address sarcopenia by improving issues related to mitochondrial function.
- Blood flow restriction training (BFRT): BFRT involves using a special device to apply pressure to the upper part of the muscles, limiting blood flow during exercise. Originating in Japan, it is also known as “KAATSU training,” meaning “adding pressure to training.” It is typically done at low intensity and effectively reduces muscle wasting, improves muscle mass, and boosts strength. As a result, it is considered an effective treatment for sarcopenia in clinical practice.
2. Diet
Increasing protein intake through food or supplements can help prevent and manage sarcopenia. Protein is essential for building muscle, as the body breaks it down into amino acids used to repair and grow muscle tissue. Consuming 20 to 35 grams of protein per meal supports muscle protein synthesis, combating muscle loss. A daily intake of 1.0 to 1.2 grams per kilogram of body weight is recommended for sarcopenic patients.3. Potential Treatments
The U.S. Food and Drug Administration (FDA) has not approved any pharmacological treatments for sarcopenia yet, but new therapies are in development. Selective androgen receptor modulators (SARMs) are promising due to their tissue selectivity. Other potential treatments under investigation include myostatin inhibitors, ACE inhibitors, omega-3 supplements, and anabolic agents such as ghrelin and its analogs.How Does Mindset Affect Sarcopenia?
What Are the Natural Approaches to Sarcopenia?
1. Supplements
- Vitamin D: Low vitamin D levels are linked to an increased risk of sarcopenia in older adults. Vitamin D deficiency primarily affects the lower limb muscles, crucial for balance and walking, and is associated with a higher risk of falls. Supplementing with vitamin D has been shown to improve hand grip strength in postmenopausal women, lower limb strength in athletes, and hip muscle strength in people 40 years old and older.
- Omega-3 fatty acids: Supplementing with dietary omega-3 fatty acids enhances muscle anabolic signaling. A 2015 study showed that fish oil-derived omega-3 polyunsaturated fatty acid (PUFA) therapy significantly enhanced muscle anabolism (a process that bonds cells) and physical performance in older adults. A 2011 study also found that omega-3 fatty acid supplements boosted the insulin–amino acid-induced increase in muscle protein synthesis in older adults.
- Creatine monohydrate (CrM): When performing resistance exercises, skeletal muscles produce creatine monohydrate, a key energy source that helps sustain strong muscle contractions. As per a 2024 study, CrM supplements, combined with resistance exercise, improved cholesterol levels, reduced inflammation, and counteracted age-related oxidative stress in a rat model. This combination enhances muscle strength and endurance by supporting cellular energy production and reducing inflammation. The study also demonstrated that CrM and resistance exercise together improved muscle performance and overall health, suggesting a potential to support healthy aging and muscle longevity in humans.
- Nicotinamide adenine dinucleotide (NAD+): Nicotinamide adenine dinucleotide is a coenzyme essential for cell energy production, supporting processes such as DNA repair, aging, and immune responses. Research in aging mouse models shows that boosting the NAD+ salvage pathway (which sustains NAD+) can help improve sarcopenia by restoring muscle stem cells. NAD+ precursors, including oral nicotinamide riboside, nicotinamide mononucleotide, and niacin—all of which are forms of vitamin B3—have been shown to help protect against age-related muscle diseases in humans or rodents. The NAD+ pathway has therapeutic potential for treating sarcopenia by reversing the damaging processes that contribute to muscle loss. Research on the effects of NAD+ on humans is ongoing.
2. Leucine Administration
Leucine, an essential amino acid, provides energy to skeletal muscles during exercise. In a 2020 study, older participants received either leucine (6 grams per day) or lactose, a milk sugar (6 grams per day), for 13 weeks. Leucine was well-tolerated and significantly improved sarcopenia criteria, including walking performance, lean mass index, and respiratory muscle function, compared to placebo.3. Qigong
A 2017 randomized study of 65 adults found that practicing yi jin jing (sinew-transforming qigong exercises) for 12 weeks significantly improved muscle strength in older adults with sarcopenia, while no improvement was seen in a control group without training. The difference between the two groups was statistically significant, demonstrating that consistent yi jin jing practice can effectively enhance skeletal muscle strength in aging adults.4. Electrical Acupuncture
A 2018 study involving 48 older men with sarcopenic obesity tested two treatments: electrical acupuncture combined with oral essential amino acids and oral essential amino acids alone. Both groups showed improvements in body fat percentage and muscle mass over 28 weeks, but the first group had faster results. After 12 weeks, the first group showed significant improvements in muscle mass, while the second group only showed changes after 28 weeks.Promising Animal Studies
- Go-sha-jinki-gan (GJG): Go-sha-jinki-gan, a traditional Japanese herbal medicine composed of paeoniflorin (derived from tree peony bark), loganin (derived from Rehmannia glutinosa root), and total alkaloids (from processed aconite root), has been found to help with age-related sarcopenia. In a 2015 study using aged mice, GJG significantly reduced muscle mass loss and prevented aging-related changes in muscle fiber types. It also improved key molecular processes related to muscle health and energy production, bringing these closer to levels seen in healthier, younger mice. Therefore, GJG may be an effective treatment for sarcopenia in the future.
- Ninjin’yoeito (ren shen yang ying tang): According to a 2018 study, ninjin’yoeito is a powerful traditional Japanese medicine made from 12 natural ingredients, including ginseng, cinnamon bark, and peony root. It has been shown to improve appetite, reduce age-related sarcopenia, and extend lifespan in aging mouse models. The researchers suggested that these models indicate that ninjin’yoeito may slow the effects of aging and improve overall health.
- Ishige okamurae: A 2022 study found Ishige okamurae, an edible brown seaweed, and its active compound diphloroethohydroxycarmalol (DPHC) help restore muscle health and combat age-related sarcopenia in a mouse model. In aging mice, Ishige okamurae extract and DPHC improved muscle regeneration, increased lean muscle mass, and enhanced exercise ability by addressing hormonal imbalances and aging-related muscle damage.
How Can I Prevent Sarcopenia?
- Staying physically active: Regular physical activity is essential for preventing sarcopenia. Resistance training has been shown to positively affect the neuromuscular system, hormone levels, and protein synthesis. Combining resistance (strength) training with aerobic exercise helps develop and preserve muscle mass.
- Optimizing nutrition: Consuming enough protein from lean meats, fish, eggs, dairy, legumes, and nuts helps repair and build muscle tissue. Try to get 20 to 35 grams of protein with each meal. Ensure adequate vitamin D intake through sunlight, fortified foods, or supplements to support muscle function, and include omega-3 fatty acids from sources such as fatty fish, flaxseeds, and walnuts to reduce inflammation and promote muscle health. Additionally, avoid pro-inflammatory processed foods and eat antioxidant-rich whole foods, like colorful fruits and vegetables. Antioxidants help the body counter oxidative stress, which aggravates sarcopenia.
- Managing underlying conditions: Chronic conditions such as diabetes, arthritis, high blood pressure, and hormonal imbalances can contribute to sarcopenia by piling on to the body’s stress load. Making appointments for regular checkups will help you monitor muscle health and identify early signs of sarcopenia.
- Considering supplements: Supplements may be beneficial if you cannot meet your nutritional needs through diet alone. Consult your doctor to determine if you need whey protein, essential amino acids such as leucine, or vitamin D supplements.
- Avoiding smoking: Smoking more than doubles a person’s chances of developing sarcopenia.
- Managing stress: Anything that adds to the body’s oxidative stress load, including mental stress, can contribute to inflammation and accelerate aging.
- Keeping a consistent sleep schedule: Sleep helps the body detoxify and fight oxidative stress. Aim to get seven or eight hours of sleep per night.
- Avoiding toxins: Drinking excessive alcohol, air pollution, and other environmental toxins contribute to oxidative stress, aggravating sarcopenia.
- Hydrating: Drinking water helps flush the system of toxins that accumulate and promote premature aging.