Researchers from Iowa State University have found that dietary zinc supplements may help prevent bacteria from sharing antimicrobial resistance (AMR) genes, potentially offering a new approach against a growing global public health threat.
“We have been treating bacterial infections with antibiotics for many years, but we are now facing the emergence of antimicrobial resistance, including resistance to the last-resort antibiotics we’ve developed,” Melha Mellata, a microbiologist at Iowa State University and senior author of the study, told The Epoch Times. “Unfortunately, we are not developing new antibiotics at a sufficient rate because when we create an antibiotic, bacteria inevitably adapt and become resistant.”
How Zinc Blocks Resistance
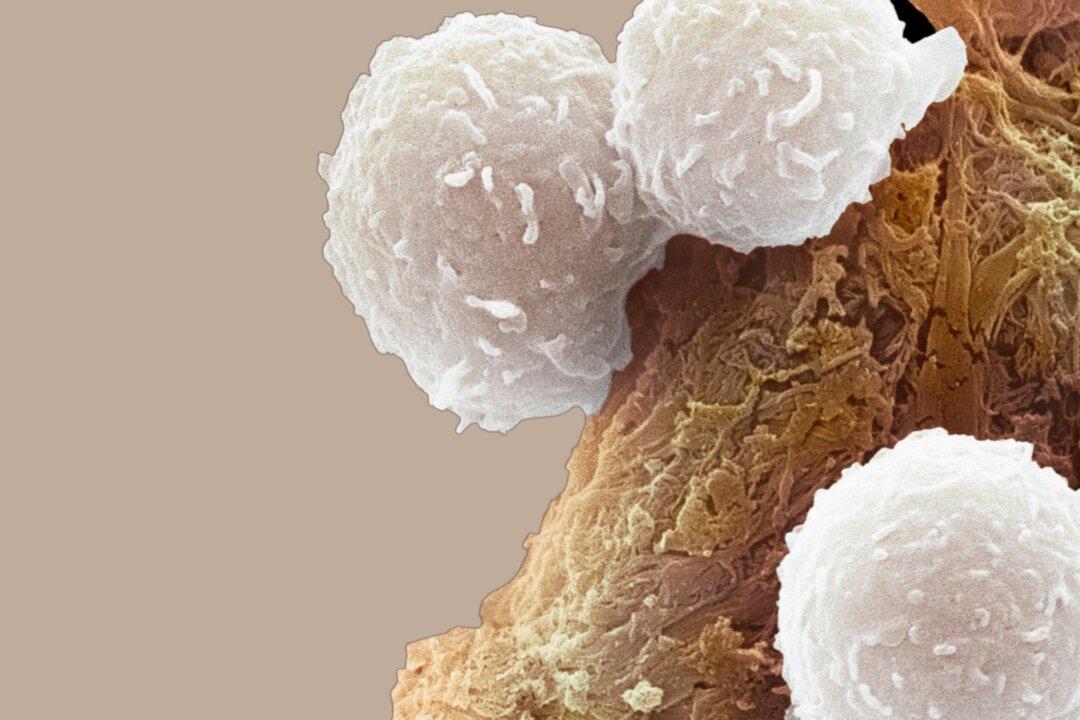
Published in Applied and Environmental Microbiology, the study highlights zinc’s role in preventing the transfer of AMR plasmids—circular DNA molecules that carry antibiotic-resistance genes—between bacteria.“We are exploring vaccines, but with the strains I’m studying, they not only carry antibiotic resistance but also virulence genes,” Mellata said. “This means we are also dealing with new bacteria that have new virulence traits. Some of these bacteria are becoming more systemic and more deadly.”
A particularly concerning aspect of AMR is that bacteria can share resistance genes, meaning patients may be resistant to multiple antibiotics before treatment even begins.
This is the first study to demonstrate zinc’s ability to prevent AMR plasmid transfer between bacteria, Mellata said. Unlike antibiotics, zinc supplementation at low doses doesn’t appear to harm beneficial gut bacteria.
“We need to educate health care professionals about this approach,” she said. “It takes time, but scientists are the first to discover something new.”
From Observation to Discovery
The current study was sparked by prior experiments in Mellata’s lab examining the effects of probiotics and a live Salmonella vaccine on the gut microbiome of chickens.“We observed that when we combined the vaccine with probiotics, there were significantly fewer bacteria containing plasmids with antimicrobial resistance,” Mellata said. This observation prompted the team to investigate other oral interventions, including dietary supplements.
Laboratory Findings Show Promise
Logan Ott, the new study’s lead researcher, directed a team of undergraduate students in testing various supplements’ ability to inhibit plasmid transmission.They conducted experiments using avian pathogenic Escherichia coli (E. coli) with multidrug-resistant plasmids, testing their interactions with a plasmid-free human E. coli.
Next Steps in Research
The research team plans to expand their investigation by testing additional AMR genes, conducting animal model experiments, and verifying whether laboratory results translate to living organisms.In the past, Mellata and her team focused on targeting bacteria directly, but her “recent research highlights the importance of gut microbiota in overall health,” she noted. Disrupting the gut microbiome with antibiotics can lead to additional health issues—a fact familiar to anyone who has experienced antibiotic-related digestive problems, Mellata added.
A New Approach to an Urgent Crisis
The study offers hope in the ongoing battle against AMR. It suggests that approaches focused on inhibiting gene transmission rather than outright elimination of all gut bacteria may provide a viable pathway to preserve gut health while combating an urgent health crisis.According to Mellata, given the growing threat of AMR, innovative solutions like this could be essential in altering the trajectory of infection treatment and prevention in the future.
“By removing these resistance genes, we can solve the antibiotic efficacy problem [and] allow antibiotics to work as intended,” Mellata said. “We could save a lot of money and, more importantly, save lives.”