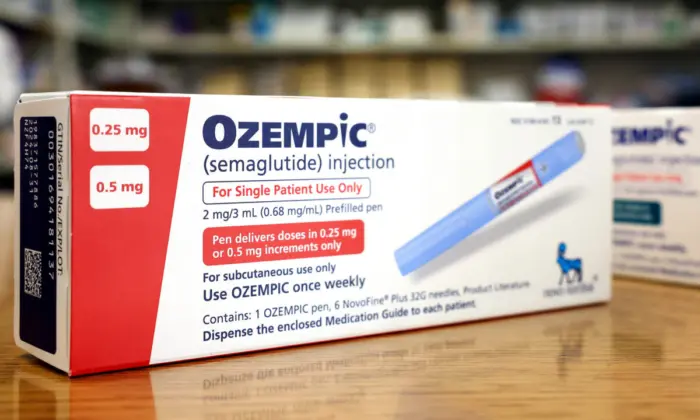
The use of prescription drugs for weight loss has been controversial, and it is essential to consult with a doctor before considering their use. Two medications in particular—Wegovy and Ozempic—have skyrocketed in popularity over the last few years. Despite their fame, these medications can have potential risks and side effects that need to be evaluated by a qualified professional.
Mounjaro, made by American pharmaceutical company Eli Lilly, has tirzepatide as its active substance, which works similarly to semaglutide by acting as two hormones, glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide 1 (GLP-1).
What Doctors Say
Semaglutide and tirzepatide are considered “safe and effective,” Dr. Harold Bays, the medical director and president of the Louisville Metabolic and Atherosclerosis Research Center, told The Epoch Times. “If you look at the clinical trial evidence, what I would say is that both semaglutide and tirzepatide improve not just the weight of patients, but the health of patients.” Bays is also the chief science officer of the Obesity Medicine Association and has contributed to studies related to Wegovy.The study also showed decreased waist circumference, BMI, blood pressure, and blood glucose levels.
Weight Loss, or Muscle Loss?
Dr. Robert Lustig, director of the Weight Assessment for Teen and Child Health Program at the University of California, San Francisco, pointed out that in the same study, 40 percent of the weight lost was lean mass, and many side effects were reported. Lean mass is the total body weight minus body fat weight. Since the weight of organs, skin, and bones won’t change much, body water and muscle mass are the two significant parts of lean mass to look at during weight loss.“That’s what starvation does,“ he said recently at the STAT Breakthrough Summit in San Francisco. ”You lose equal amounts of muscle and fat,” he added. “If you’re a person 60 years old or over and you’re losing muscle, your risk of dying just went up exponentially.”
Losing muscle during weight loss is not considered desirable because muscle keeps you strong and fit. In addition, losing muscle can slow metabolism, which means the body will burn fewer calories.
Relying Solely on Medication Is Not Healthy
“There is healthy weight loss and unhealthy weight loss,” Dr. Konstantinos Spaniolas, director of the Bariatric and Metabolic Weight Loss Center at Stony Brook University, told The Epoch Times.“Overall, the medications are safe,” Spaniolas said. But he noted that they need to be used in the right setting, alongside proper nutritional coaching, for long-lasting benefits.
Bays echoed Spaniolas’ concerns and emphasized that medications should not be the sole means of losing weight. “It should not be assumed that all the effectiveness of managing obesity should be left up to the effects of the drug,” Bays said. “I don’t think that’s the right way to go.”
Concerns About Side Effects and How the Medication Works
The 2021 clinical trial revealed a high incidence of gastrointestinal problems—such as nausea, diarrhea, vomiting, and constipation—in just over 74 percent of participants taking semaglutide, compared to nearly 48 percent receiving a placebo.Some experts reject these drugs entirely due to their side effects and the working mechanism.
Lauren Muhlheim, a certified eating disorder specialist and clinical psychologist, told The Epoch Times that taking these drugs could lead to eating disorders. “They essentially operate on the same mechanism as an eating disorder,” she added, as the drugs work by reducing appetite and causing people to undereat.
As a result, people tend to lose weight because they eat less, not because the drugs magically burn fat, Muhlheim said. In addition, individuals who are not eating enough may binge eat later and are at risk of developing anorexia.
High Cost and Risks Associated With Regained Weight
Muhlheim cited research indicating that weight loss achieved by taking semaglutide is only temporary. The study, published in 2022 in Diabetes, Obesity and Metabolism, found that people who stopped taking semaglutide regained two-thirds of the lost weight in one year. Furthermore, improvements in cardiometabolic complications, such as type 2 diabetes and high blood pressure, also reversed.Conflict of Interest
The 2021 study demonstrating the benefits of semaglutide was supported by the drug’s manufacturer, Novo Nordisk. “There’s a lot of conflicts of interest that need to be considered,” Muhlheim said. “People should remember that drug companies are more interested in profit than the health of larger-bodied people and that larger-bodied people are a target for profit.”Bays, who helped run the 2021 study and has received funds from Novo Nordisk, said that anti-obesity medication clinical trials are often funded by their manufacturers.
“Unless the data is fraudulent, the raw results of these clinical trials would not be expected to change, no matter the funding,” Bays added. He also noted that several anti-obesity medication initiatives had been withdrawn due to safety or efficacy problems, regardless of whether the manufacturer funded the clinical trials.