Abstract
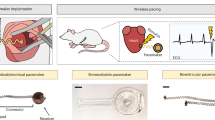
Temporary pacemakers are essential for the care of patients with short-lived bradycardia in post-operative and other settings1,2,3,4. Conventional devices require invasive open-heart surgery or less invasive endovascular surgery, both of which are challenging for paediatric and adult patients5,6,7,8. Other complications9,10,11 include risks of infections, lacerations and perforations of the myocardium, and of displacements of external power supplies and control systems. Here we introduce a millimetre-scale bioresorbable optoelectronic system with an onboard power supply and a wireless, optical control mechanism with generalized capabilities in electrotherapy and specific application opportunities in temporary cardiac pacing. The extremely small sizes of these devices enable minimally invasive implantation, including percutaneous injection and endovascular delivery. Experimental studies demonstrate effective pacing in mouse, rat, porcine, canine and human cardiac models at both single-site and multi-site locations. Pairing with a skin-interfaced wireless device allows autonomous, closed-loop operation upon detection of arrhythmias. Further work illustrates opportunities in combining these miniaturized devices with other medical implants, with an example of arrays of pacemakers for individual or collective use on the frames of transcatheter aortic valve replacement systems, to provide unique solutions that address risks for atrioventricular block following surgeries. This base technology can be readily adapted for a broad range of additional applications in electrotherapy, such as nerve and bone regeneration, wound therapy and pain management.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data supporting the results of this study are present in the paper and Supplementary Information. Source data are provided with this paper.
Code availability
The code for connecting to the device via BLE, recording and analysing ECG data in real time, and configuring the pacing parameters in a closed-loop system is available on Code Ocean at https://codeocean.com/capsule/9406347/tree/v1 (ref. 49).
References
Choi, Y. S. et al. Fully implantable and bioresorbable cardiac pacemakers without leads or batteries. Nat. Biotechnol. 39, 1228–1238 (2021).
Zhang, Y. et al. Advances in bioresorbable materials and electronics. Chem. Rev. 123, 11722–11773 (2023).
Choi, Y. S. et al. A transient, closed-loop network of wireless, body-integrated devices for autonomous electrotherapy. Science 376, 1006–1012 (2022).
Lumia, F. J. & Rios, J. C. Temporary transvenous pacemaker therapy: an analysis of complications. Chest 64, 604–608 (1973).
Wood, M. A. & Ellenbogen, K. A. Cardiac pacemakers from the patient’s perspective. Circulation 105, 2136–2138 (2002).
Bar-Cohen, Y. et al. Minimally invasive implantation of a micropacemaker into the pericardial space. Circ. Arrhythm. Electrophysiol. 11, e006307 (2018).
Zhao, J. et al. Permanent epicardial pacing in neonates and infants less than 1 year old: 12-year experience at a single center. Transl. Pediatr. 11, 825–833 (2022).
Wildbolz, M., Dave, H., Weber, R., Gass, M. & Balmer, C. Pacemaker implantation in neonates and infants: favorable outcomes with epicardial pacing systems. Pediatr. Cardiol. 41, 910–917 (2020).
Wilhelm, M. J. et al. Cardiac pacemaker infection: surgical management with and without extracorporeal circulation. Ann. Thorac. Surg. 64, 1707–1712 (1997).
Donovan, K. D. & Lee, K. Y. Indications for and complications of temporary transvenous cardiac pacing. Anaesth. Intensive Care 13, 63–70 (1985).
BRAUN, M. U. et al. Percutaneous lead implantation connected to an external device in stimulation-dependent patients with systemic infection—a prospective and controlled study. Pacing Clin. Electrophysiol. 29, 875–879 (2006).
Ouyang, H. et al. Symbiotic cardiac pacemaker. Nat. Commun. 10, 1821 (2019).
Lyu, H. et al. Synchronized biventricular heart pacing in a closed-chest porcine model based on wirelessly powered leadless pacemakers. Sci. Rep. 10, 2067 (2020).
Ho, J. S. et al. Wireless power transfer to deep-tissue microimplants. Proc. Natl Acad. Sci. USA 111, 7974–7979 (2014).
Wang, S. et al. A self-assembled implantable microtubular pacemaker for wireless cardiac electrotherapy. Sci. Adv. 9, eadj0540 (2023).
Prominski, A. et al. Porosity-based heterojunctions enable leadless optoelectronic modulation of tissues. Nat. Mater. 21, 647–655 (2022).
Liu, Z. et al. Photoelectric cardiac pacing by flexible and degradable amorphous Si radial junction stimulators. Adv. Healthc. Mater. 9, 1901342 (2020).
Wang, L. et al. A fully biodegradable and self-electrified device for neuroregenerative medicine. Sci. Adv. 6, eabc6686 (2020).
Zhang, Y. et al. Self-powered, light-controlled, bioresorbable platforms for programmed drug delivery. Proc. Natl. Acad. Sci. USA 120, e2217734120 (2023).
Huang, I. et al. High performance dual-electrolyte magnesium–iodine batteries that can harmlessly resorb in the environment or in the body. Energy Environ. Sci. 15, 4095–4108 (2022).
Won, S. M. et al. Natural wax for transient electronics. Adv. Funct. Mater. 28, 1801819 (2018).
Choi, Y. S. et al. Biodegradable polyanhydrides as encapsulation layers for transient electronics. Adv. Funct. Mater. 30, 2000941 (2020).
Song, G. Control of biodegradation of biocompatable magnesium alloys. Corros. Sci. 49, 1696–1701 (2007).
Schauer, A. et al. Biocompatibility and degradation behavior of molybdenum in an in vivo rat model. Materials 14, 7776 (2021).
Yin, L. et al. Dissolvable metals for transient electronics. Adv. Funct. Mater. 24, 645–658 (2014).
Yu, K. J. et al. Bioresorbable silicon electronics for transient spatiotemporal mapping of electrical activity from the cerebral cortex. Nat. Mater. 15, 782–791 (2016).
Kang, S.-K. et al. Bioresorbable silicon electronic sensors for the brain. Nature 530, 71–76 (2016).
Li, G. et al. Flexible transient phototransistors by use of wafer‐compatible transferred silicon nanomembranes. Small 14, e1802985 (2018).
Li, G. et al. Silicon nanomembrane phototransistor flipped with multifunctional sensors toward smart digital dust. Sci. Adv. 6, eaaz6511 (2020).
López Ayerbe, J. et al. Temporary pacemakers: current use and complications. Rev. Esp. Cardiol. Engl. Ed. 57, 1045–1052 (2004).
Yu, L., Nina-Paravecino, F., Kaeli, D. & Fang, Q. Scalable and massively parallel Monte Carlo photon transport simulations for heterogeneous computing platforms. J. Biomed. Opt. 23, 1 (2018).
Fang, Q. & Boas, D. A. Monte Carlo simulation of photon migration in 3D turbid media accelerated by graphics processing units. Opt. Express 17, 20178 (2009).
Taroni, P., Pifferi, A., Torricelli, A., Comelli, D. & Cubeddu, R. In vivo absorption and scattering spectroscopy of biological tissues. Photochem. Photobiol. Sci. 2, 124–129 (2003).
Khan, R., Gul, B., Khan, S., Nisar, H. & Ahmad, I. Refractive index of biological tissues: review, measurement techniques, and applications. Photodiagnosis Photodyn. Ther. 33, 102192 (2021).
Green, M. A. & Keevers, M. J. Optical properties of intrinsic silicon at 300 K. Prog. Photovoltaics Res. Appl. 3, 189–192 (1995).
Firbank, M., Hiraoka, M., Essenpreis, M. & Delpy, D. T. Measurement of the optical properties of the skull in the wavelength range 650–950 nm. Phys. Med. Biol. 38, 503–510 (1993).
Rahko, P. S. Evaluation of the skin-to-heart distance in the standing adult by two-dimensional echocardiography. J. Am. Soc. Echocardiogr. 21, 761–764 (2008).
Chen, R. et al. Deep brain optogenetics without intracranial surgery. Nat. Biotechnol. 39, 161–164 (2021).
Yin, R. T. et al. Open thoracic surgical implantation of cardiac pacemakers in rats. Nat. Protoc. 18, 374–395 (2023).
Yang, Q. et al. Photocurable bioresorbable adhesives as functional interfaces between flexible bioelectronic devices and soft biological tissues. Nat. Mater. 20, 1559–1570 (2021).
Shea, J. B. & Sweeney, M. O. Cardiac resynchronization therapy a patient’s guide. Circulation 108, e64–e66 (2003).
Connolly, S. J., Kerr, C., Gent, M. & Yusuf, S. Dual-chamber versus ventricular pacing. Circulation 94, 578–583 (1996).
Rodés-Cabau, J., Muntané-Carol, G. & Philippon, F. Managing conduction disturbances after TAVR: toward a tailored strategy. JACC Cardiovasc. Interv. 14, 992–994 (2021).
Urena, M. & Rodés-Cabau, J. Conduction abnormalities: the true Achilles’ heel of transcatheter aortic valve replacement? JACC Cardiovasc. Interv. 9, 2217–2219 (2016).
Pagnesi, M. et al. Incidence, predictors, and prognostic impact of new permanent pacemaker implantation after TAVR with self-expanding valves. JACC Cardiovasc. Interv. 16, 2004–2017 (2023).
Reiter, C. et al. Delayed total atrioventricular block after transcatheter aortic valve replacement assessed by implantable loop recorders. JACC Cardiovasc. Interv. 14, 2723–2732 (2021).
Muntané-Carol, G. et al. Ambulatory electrocardiographic monitoring following minimalist transcatheter aortic valve replacement. JACC Cardiovasc. Interv. 14, 2711–2722 (2021).
Krishnaswamy, A. et al. Feasibility and safety of same-day discharge following transfemoral transcatheter aortic valve replacement. JACC Cardiovasc. Interv. 15, 575–589 (2022).
Millimetre-scale, bioresorbable optoelectronic systems for minimally invasive electrotherapy. Code Ocean https://codeocean.com/capsule/9406347/tree/v1 (2025).
Acknowledgements
We acknowledge support from the Querrey Simpson Institute for Bioelectronics, the Leducq Foundation grant ‘Bioelectronics for Neurocardiology’ and the NIH grant (NIH R01 HL141470). Y.Z. acknowledges support from the National University of Singapore start-up grant and the AHA’s Second Century Early Faculty Independence Award (grant: https://doi.org/10.58275/AHA.23SCEFIA1154076.pc.gr.173925). J. Gong and Z.M. acknowledge the support from AFOSR (grant number FA9550-21-1-0081). We thank E. Dempsey, Q. Ma, N. Ghoreishi-Haack, I. Stepien and S. Han for the help in the biocompatibility study and animal experiment. This work made use of the NUFAB facility of Northwestern University’s NUANCE Center, which has received support from the SHyNE Resource (NSF ECCS-2025633), the IIN and Northwestern’s MRSEC programme (NSF DMR-1720139). This work was supported by the Developmental Therapeutics Core and the Center for Advanced Molecular Imaging (RRID:SCR_021192) at Northwestern University and the Robert H. Lurie Comprehensive Cancer Center support grant (NCI P30 CA060553).
Author information
Authors and Affiliations
Contributions
Y.Z. and J.A.R. initiated and conceived the self-powered, light-controlled pacing concept. Y.Z., E.R., I.R.E. and J.A.R. designed the studies and analysed the results. Y.Z., L.Z., K.Z., X.L., A.L., G.J., J.L., F.L., Y.F.L.L., Y.L., C.H., A.H. and R.N. fabricated and characterized the pacemakers. E.R., L.T., A. Mikhailov, L.D., A.B., A.P., A.A. and A. Melisova conducted animal surgeries. Y.Z., E.R., L.Z., L.T., A. Mikhailov, L.D., J.W., A.B., A.P. and W.O., performed in vivo and ex vivo cardiac pacing experiments. W.O., Y.W., J. Gu, T.Y., Y.Y. and Y.L. developed closed-loop and optical control systems. J.U.K., S.G.S., J. Gong, J.J., J.C., S.H.J. and Z.M. designed and fabricated phototransistors. H.Z., S.L., Z.L. and Y.H. performed computational simulations. E.A. and W.B. fabricated bioresorbable optical filters. T.W., N.S.P. and J.M.T. developed and synthesized the hydrogels. L.T., L.D. and K.B. evaluated the biocompatibility. Y.Z., E.R., L.Z., J.U.K., L.T., A. Mikhailov., K.Z., X.L., Y.W., H.Z., A.L., E.A., G.J., S.L., S.G.S., K.B., N.L., W.O., R.K.A., I.R.E. and J.A.R. discussed and interpreted the data. Y.Z. and J.A.R. prepared figures and wrote the paper, with input from E.R., W.O., A. Mikhailov, R.K.A. and I.R.E. In addition, J.U.K., L.Z., L.T., Y.W., H.Z., S.L. and J. Gu. assisted with the preparation of figures and text. Y.Z., L.Z., L.T., H.Z., L.D., W.O., I.R.E. and J.A.R. revised the paper. Y.Z., E.R., L.Z., J.U.K., L.T. and H.Z. contributed equally to this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks Gábor Duray, Hossam Haick and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Comparisons of previously reported pacemakers and the technology introduced here.
a, Comparisons between conventional pacemakers with leads, leadless pacemakers, bioresorbable pacemakers, and the pacemaker reported here. b, Table showing details of previously reported leadless pacemakers and the pacemaker reported here. Illustration of the pacemaker with leads in a was created with BioRender.com (https://biorender.com). Bioresorbable pacemaker in a adapted from ref. 1, Springer Nature America, Inc.
Extended Data Fig. 2 Characteristics of bipolar junction transistor (BJT)-based phototransistors.
a,b, Characteristic curves of the phototransistors under various light intensities emitted from a NIR LED (850 nm, a) and a red LED (650 nm, b).
Extended Data Fig. 3 Measurement of the operational lifespan of the device.
a, EIS of an agarose gel and chicken tissue. b, The output currents of the pacemaker over days. c, Output currents of the pacemaker over days under pulsed illumination.
Extended Data Fig. 4 In vivo demonstration of cardiac pacing in mouse models.
a, Photograph showing a pacemaker placed on the surface of a mouse heart. b, ECG results before and during mouse heart pacing. c, Strength-duration curve when pacing at 480 bpm. n = 3 biologically independent animals.
Extended Data Fig. 5 Selection of LEDs and optical filters for multi-site, time-synchronized cardiac pacing.
a, Emission spectra for LEDs 1 and 2. b, Transmission curves for filters 1 and 2. c, Transmitted light intensities as a function of incident intensities from LEDs 1 and (2) for filters 1 and 2.
Supplementary information
Supplementary Information
Supplementary Methods, Notes 1–11, Tables 1–3, Figs. 1–26 and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Rytkin, E., Zeng, L. et al. Millimetre-scale bioresorbable optoelectronic systems for electrotherapy. Nature 640, 77–86 (2025). https://doi.org/10.1038/s41586-025-08726-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-025-08726-4
This article is cited by
-
Materials and device strategies to enhance spatiotemporal resolution in bioelectronics
Nature Reviews Materials (2025)
-
Development of a miniature, bioresorbable, light-activated pacemaker
Nature Reviews Cardiology (2025)